What an Anaphylaxis Action Plan Really Is
An anaphylaxis action plan isn’t just a piece of paper. It’s a clear, step-by-step emergency guide that tells exactly what to do when someone has a life-threatening allergic reaction. This isn’t theoretical. Every year, dozens of people in schools and workplaces die because the right thing wasn’t done fast enough. The plan cuts through confusion. It says: epinephrine first. No waiting. No second-guessing. No asking permission.
These plans are built on standards from the CDC, FARE, and the Asthma and Allergy Foundation of America. They’re not suggestions. They’re the minimum expected response when someone’s airway is closing, their blood pressure is dropping, or they’re losing consciousness. In schools, they’re legally required in 49 states. In workplaces, they’re often missing - and that’s deadly.
What’s Actually in the Plan? (No Guesswork Allowed)
A real anaphylaxis action plan has five non-negotiable parts:
- Photo ID - A clear picture of the person with allergies. This isn’t for bureaucracy. It’s so anyone can recognize them instantly during a panic.
- Confirmed allergens - Not ‘might be allergic to peanuts.’ Not ‘probably sensitive to shellfish.’ It must say: ‘Allergic to tree nuts, specifically cashews and walnuts.’ Exact names. No room for error.
- Symptom checklist - Mild symptoms? Hives, itching, swelling, runny nose. Severe symptoms? Wheezing, throat tightness, dizziness, vomiting, fainting. The plan doesn’t say ‘if it looks bad.’ It says: ‘If two body systems are affected - give epinephrine now.’
- Epinephrine instructions - This is the most important part. The plan must say: ‘Administer epinephrine immediately.’ No ‘if you’re unsure.’ No ‘wait and see.’ If the person has trouble breathing or their skin turns pale, it’s time. Delayed epinephrine increases death risk by 83%.
- Emergency contacts - Parent, guardian, doctor. Not just a number. A name, relationship, and phone. And a backup contact if the first one doesn’t answer.
Every plan must be signed by a doctor. No exceptions. A school nurse can’t sign it. A manager can’t sign it. Only a licensed medical provider can confirm the diagnosis and the treatment plan.
Why Schools Are Getting It Right - Mostly
Most U.S. schools have anaphylaxis plans because the law forces them to. The CDC’s 2020 guidelines became the national standard. Now, 49 states require schools to have written emergency procedures. Forty states allow stock epinephrine - meaning even if a student doesn’t have their own injector, the school keeps two on hand.
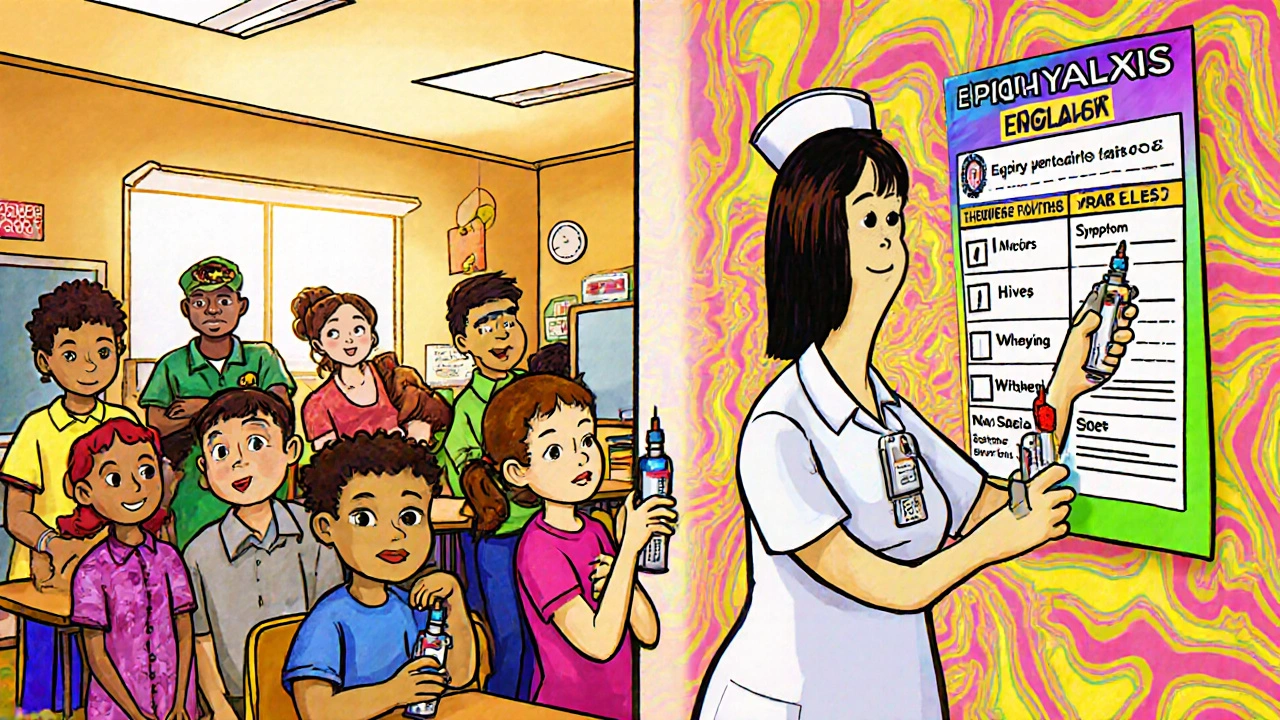
Successful schools don’t just hand out forms. They train. They practice. They test.
- At least two staff members per classroom are trained to use an epinephrine auto-injector. That’s the NASN recommendation. Only 61% of schools meet that.
- Training isn’t a one-time thing. It’s 90 minutes at the start of the year, then 60 minutes every year after. Only 37% of schools do annual refreshers.
- Epinephrine isn’t locked in a cabinet. It’s in a clear, labeled bag, in a place everyone knows - the nurse’s office, the main office, the cafeteria. New York’s 2024 rules say it must be reachable in 60 seconds.
When these steps are followed, success rates jump. A 2023 AAFA survey found 65% of schools with standardized plans had full, successful responses to reactions. In schools with random, hand-written notes? Only 28%.
Workplaces Are Falling Behind - And People Are Getting Hurt
Workplaces don’t have the same rules. There’s no federal mandate. Only 28 states have any specific anaphylaxis policy for employers. That means it’s up to the boss - and most bosses don’t know what to do.
Here’s what happens in real workplaces:
- A server with a shellfish allergy keeps their epinephrine in their bag - but their manager says it can’t be kept near the food prep area. During a reaction, they have to run to the bathroom to use it.
- A warehouse worker has a peanut allergy. When they start to wheeze, no one knows where the injector is. No one was trained. They wait 12 minutes before calling 911.
- A retail employee has a history of anaphylaxis. HR says they ‘can’t be responsible’ for storing medication. The employee is told to ‘just be careful.’
FARE’s 2022 survey found 57% of workers with severe allergies had at least one reaction where coworkers hesitated to help. Why? 33% said they were scared of getting sued. That’s not fear of the allergy - that’s fear of the system.
OSHA says employers must provide first aid. But they don’t say what that means for anaphylaxis. That loophole kills. The same people who know how to use a fire extinguisher don’t know how to use an EpiPen - because no one trained them.
How to Build a Real Plan - Step by Step
If you’re a school administrator, a manager, or a parent pushing for change, here’s how to get it right:
- Use the official template - Download FARE’s 2023 Anaphylaxis Action Plan. It’s free. It’s clear. It’s been used in 78% of U.S. school districts. Don’t use your district’s old, confusing form.
- Get it signed - Take it to the allergist. Make sure they fill in the exact allergens, symptoms, and epinephrine instructions. No vague language.
- Train everyone - Not just the nurse. The janitor. The bus driver. The lunch aide. The new intern. Use free videos from FARE or AAFA. Practice with training injectors. Make it part of orientation.
- Store it right - Epinephrine should be at room temperature. Not in a locked drawer. Not in a fridge. Not in a backpack. Keep it in a bright, labeled container in a central, unlocked location. Check expiration dates every month.
- Update it yearly - Allergies change. Kids grow. New foods are introduced. Plans expire. Review every January. Get a new doctor’s signature.
Don’t wait for someone to collapse before you act. If you have even one person with known allergies, you need this plan. And you need to practice it.

What’s Changing in 2025 - And What’s Coming
The rules are getting stricter - and better.
In January 2024, the CDC added new guidance for field trips, sports, and after-school programs. Schools can no longer say, ‘We don’t handle this outside the classroom.’
FARE launched a digital plan platform in March 2024. Parents can update allergens and contacts in real time. Schools get instant alerts. It’s being used in 22% of districts already.
And by 2025, the FDA may approve new epinephrine devices with voice prompts - so even someone who’s never used one before can follow clear instructions: ‘Press here. Hold for 3 seconds.’ This could be a game-changer for workplaces.
But technology won’t fix bad policy. The real progress comes when every school and every workplace treats anaphylaxis like a fire alarm - something you test, train for, and never ignore.
Why This Isn’t Optional Anymore
Dr. Robert Wood from Johns Hopkins said it best: ‘Standardized anaphylaxis action plans are now considered essential infrastructure in educational settings, comparable to AEDs for cardiac emergencies - they’re no longer optional but fundamental to student safety.’
That’s true for workplaces too. If your building has a fire extinguisher, it should have an epinephrine injector. If you train staff on CPR, you should train them on anaphylaxis. The science is clear. The tools exist. The cost of doing nothing? Lives.
Don’t wait for a tragedy to make you act. Build the plan. Train the team. Store the medicine. Update it every year. That’s not extra work. That’s basic responsibility.
Do I need an anaphylaxis action plan if someone only has mild allergies?
Yes. Allergies can escalate fast. A mild reaction to peanuts one day can turn into anaphylaxis the next. The plan isn’t just for people who’ve had severe reactions before. It’s for anyone with a confirmed allergy, even if it’s only been mild in the past. The CDC and FARE recommend treating all confirmed allergies with a full action plan.
Can anyone use an epinephrine auto-injector?
Yes. The devices are designed for non-medical people. They have simple instructions: remove cap, press against thigh, hold for 3 seconds. Training takes less than 15 minutes. Many states have Good Samaritan laws that protect anyone who gives epinephrine in good faith. The real danger isn’t using it wrong - it’s not using it at all.
What if the school or workplace refuses to implement a plan?
In schools, you have legal rights. Under Section 504 of the Rehabilitation Act, schools must accommodate students with life-threatening allergies. If they refuse, you can file a complaint with the U.S. Department of Education’s Office for Civil Rights. In workplaces, the Americans with Disabilities Act (ADA) requires employers to provide reasonable accommodations - which includes access to epinephrine and training. Document all requests in writing. If they ignore you, contact the EEOC.
How often should epinephrine be replaced?
Check the expiration date on the injector. Most last 12 to 18 months. Replace them before they expire. Don’t wait until they’re expired to order new ones - supply chains can delay. Schools and workplaces should do monthly checks. Mark the replacement date on a calendar. If the liquid inside looks cloudy or has particles, replace it immediately - even if it’s not expired.
Can a person with anaphylaxis carry their own epinephrine?
Yes - and they should. But they shouldn’t be the only source. People can forget their injector. It can get lost. It can break. That’s why schools and workplaces need stock epinephrine. A person’s own injector is their first line of defense. Stock injectors are the safety net. Both are required for full protection.

Karen Ryan 24.11.2025
I work in a daycare and we just implemented this last year. 🙌 Epinephrine kits are now in every room, not just the office. Staff training was a game-changer. My 5-year-old had a reaction last month and the aide used the EpiPen before I even got there. I’m crying typing this. Thank you for this post.
Kaylee Crosby 24.11.2025
My kid has a cashew allergy and our school had a handwritten note taped to the nurse’s door until last spring. Now they use the FARE template. Big difference. Train the cafeteria workers too. They’re the ones who see the food most. Don’t let them guess.
Terry Bell 24.11.2025
Man I wish my workplace had this. I’ve got a peanut allergy and my boss told me to "just be careful" when I asked for an EpiPen in the breakroom. Like I’m asking for a luxury. It’s not a luxury it’s a lifeline. We train people to use defibrillators but not EpiPens? That’s messed up.
Mariam Kamish 24.11.2025
This is all just performative woke safety theater. Nobody’s dying from allergies anymore. You’re overreacting. I’ve seen people panic over a crumb. It’s anxiety, not anaphylaxis.
Benjamin Gundermann 24.11.2025
Look I get it, people die. But let’s be real - most of these plans are just paper tigers. Schools say they have them but the EpiPens are locked in the principal’s office with a key only the nurse has. And the nurse? She’s busy grading papers. And the janitor? He doesn’t even know what an EpiPen looks like. We need to stop pretending paperwork fixes systemic neglect. It doesn’t. It just makes us feel better.
Rachelle Baxter 24.11.2025
I’m a nurse. And I’ve seen too many kids die because someone waited for ‘permission’ or ‘a doctor’s order.’ This isn’t opinion. This is protocol. If you don’t have a signed plan, you’re not prepared. You’re just gambling with lives. And if you’re in a workplace that won’t act? That’s negligence. Period.
Dirk Bradley 24.11.2025
The institutionalization of anaphylaxis preparedness represents a profound shift in the sociopolitical architecture of public safety. The transition from discretionary accommodation to codified, mandatory infrastructure mirrors the evolution of fire codes in the early 20th century. One cannot, in good conscience, maintain a public-facing facility without the requisite pharmacological countermeasures. The moral calculus is unambiguous.
Manish Pandya 24.11.2025
In India, we don’t have this yet. But my cousin’s son had a reaction at school and the teacher didn’t know what to do. I shared this post with his principal. Now they’re getting training. It’s slow, but it’s starting. Thanks for the clarity. This is exactly what we needed.
Adesokan Ayodeji 24.11.2025
I’m a warehouse supervisor in Texas. We got 3 EpiPens last month after my guy had a reaction. We trained everyone - the guys on the forklifts, the inventory clerks, even the temp workers. We keep them by the breakroom door. No lock. No excuses. Last week, one of the new hires used one on a coworker who was having a reaction to a snack. Saved his life. This isn’t hard. It’s just human.
Emma Hanna 24.11.2025
I’ve been waiting for someone to say this. The fact that 49 states require this in schools but workplaces are left to the whims of corporate greed is a national disgrace. Where’s the federal law? Where’s the enforcement? This isn’t a ‘nice to have’ - it’s a civil rights issue. People with allergies are being denied equal access to safe workplaces. And no one’s doing anything about it.
Patrick Goodall 24.11.2025
I’ve got a theory: this whole anaphylaxis thing is being pushed by Big Pharma. EpiPens cost $700. Who profits? The same companies that make the food additives causing the allergies. And now they’re pushing mandatory training? It’s all connected. The CDC? FARE? All funded by the same donors. Wake up.
katia dagenais 24.11.2025
I mean… I get it. But isn’t this just enabling people to be overly fearful? Like, if you’re allergic to everything, maybe you should just… not eat? Or live in a bubble? I’m not saying don’t prepare - I’m saying maybe we’re creating a culture of fragility. What about resilience? What about teaching people to manage risk instead of eliminating all risk?
Lawrence Zawahri 24.11.2025
I’ve been saying this for years. The government doesn’t care about your kid’s allergies. They care about lawsuits. That’s why they made the rules - not to save lives, but to cover their own asses. If you don’t have a plan, you get sued. If you do? You’re still not safe. They’ll still blame you. This whole system is rigged.