Cyclobenzaprine Dose Calculator
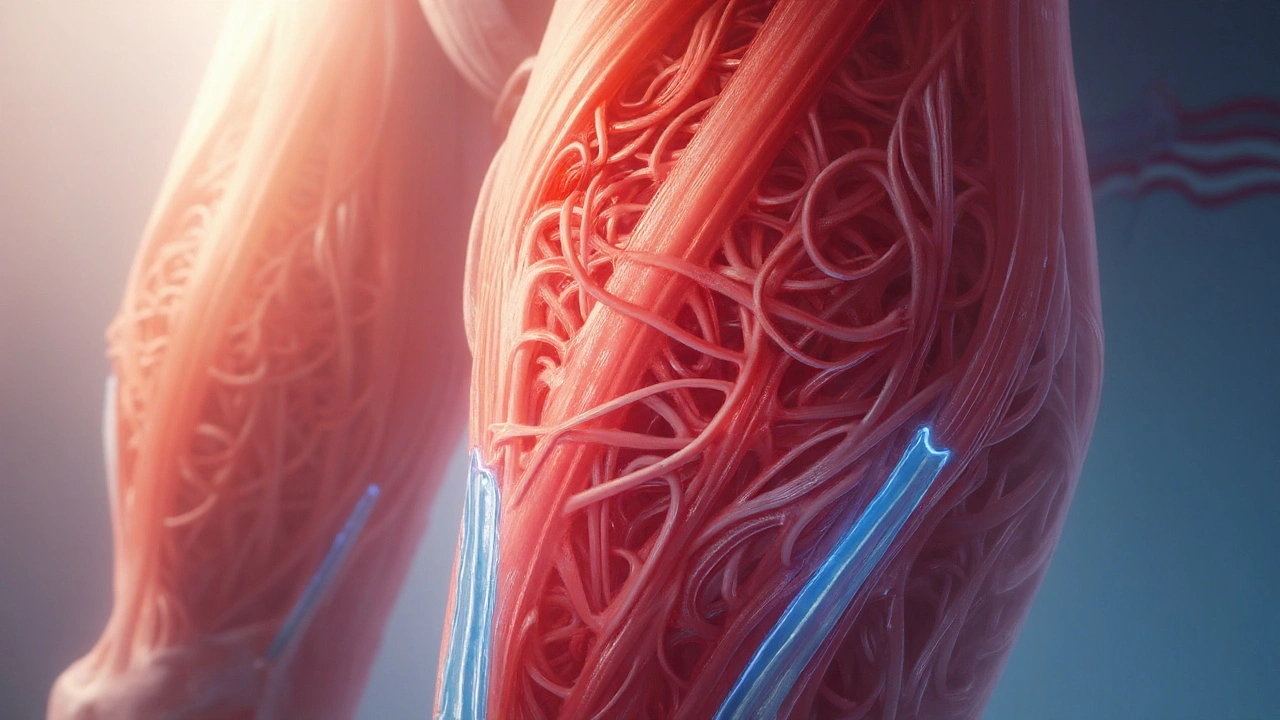
Cyclobenzaprine HCL is a centrally acting skeletal muscle relaxant that reduces muscle tone by acting on the brainstem, thereby easing post‑operative muscle spasm and associated pain.
Understanding the Mechanism
The drug’s primary target is the central nervous system, where it interrupts nociceptive pathways that cause involuntary muscle contraction. By dampening gamma‑motor neuron activity, Cyclobenzaprine allows the affected muscle groups to relax without directly acting on the muscle fibers themselves.
This indirect action distinguishes it from peripheral muscle relaxants that bind to muscle receptors. The result is a smoother transition from the acute post‑surgical phase, where guarding spasm can impede wound healing and limit early mobilisation.
Why Muscle Spasm Matters After Surgery
After an operation, the body’s natural protective response is to tighten muscles around the incision site. While this guards the wound, prolonged spasm can increase post‑operative pain, restrict range of motion, and delay physiotherapy. Studies from the American Pain Society (2023) show that uncontrolled spasm raises opioid consumption by up to 30%.
By attenuating spasm, Cyclobenzaprine helps patients start physiotherapy sooner, which correlates with faster return to daily activities and lower rates of chronic pain development.
Typical Dosage and Administration for Surgical Patients
For most adult patients, the recommended regimen is 5mg three times daily for the first week, potentially increasing to 10mg three times daily if tolerated. The drug’s half‑life averages 18hours, which supports a three‑dose schedule.
Key points to remember:
- Start within 24hours post‑operation, once the patient is alert and able to swallow.
- Avoid doses after 6pm to minimise next‑day drowsiness.
- Limit treatment to 2‑3weeks; prolonged use raises the risk of tolerance and dependence.
How Cyclobenzaprine Stacks Up Against Other Muscle Relaxants
| Drug | Onset (minutes) | Half‑Life (hours) | Typical Dose (Adult) | Sedation Level* |
|---|---|---|---|---|
| Cyclobenzaprine HCL | 30‑60 | 18 | 5‑10mg TID | Moderate |
| Methocarbamol | 45‑90 | 1‑2 | 750mg QID | Low |
| Carisoprodol | 15‑30 | 2‑3 | 350mg TID | High |
*Sedation level based on clinical consensus (2022).
When weighed against methocarbamol and carisoprodol, Cyclobenzaprine offers a longer half‑life, meaning fewer daily doses and steadier symptom control. Its moderate sedation sits between the low‑sedating methocarbamol (good for day‑time mobility) and the highly sedating carisoprodol (better for night‑time spasm). The choice ultimately hinges on patient tolerance, surgical site, and co‑prescribed analgesics.
Integrating Cyclobenzaprine With a Multimodal Pain Plan
Modern peri‑operative protocols stress multimodal analgesia-using several drug classes to hit pain pathways from different angles. Cyclobenzaprine works best when combined with:
- NSAIDs (e.g., ibuprofen 400‑600mg Q6‑8h) to curb inflammation.
- opioid analgesics for breakthrough pain, kept at the lowest effective dose.
- Early physiotherapy focusing on gentle stretching and activation.
When Cyclobenzaprine reduces spasm, patients often report needing 15‑20% less opioid in the first 48hours, lowering the risk of nausea, constipation, and respiratory depression.
Safety Profile, Side Effects, and Drug Interactions
Common adverse events include dry mouth, dizziness, and mild sedation-usually transient. Less frequent but noteworthy risks are:
- Cardiac conduction delays (especially in patients on classIA anti‑arrhythmics).
- Serotonin syndrome when combined with SSRIs, SNRIs, or tramadol.
- Exacerbation of glaucoma due to anticholinergic activity.
Key contraindications:
- Known hypersensitivity to Cyclobenzaprine or its salts.
- Recent myocardial infarction or unstable angina.
- Severe hepatic impairment (dose reduction required).
Always review the patient’s medication list for potential drug interactions. For instance, concurrent use of MAO inhibitors within 14days can precipitate hypertensive crises.
Practical Tips for Patients and Clinicians
For clinicians:
- Screen for contraindications before prescribing.
- Start at 5mg TID; titrate only if side effects are mild.
- Schedule the last dose before 6pm to protect sleep quality.
- Document any concurrent serotonergic agents and assess risk.
- Educate patients on avoiding alcohol-a synergistic depressant.
For patients:
- Take the medicine with food to lessen stomach upset.
- Report persistent dizziness or vision changes immediately.
- Combine the drug with gentle stretching as advised by the physiotherapist.
- Do not abruptly stop after a week; taper if therapy exceeds three weeks.
By following these steps, Cyclobenzaprine can become a smooth bridge between the operating room and full recovery.
Related Concepts and Next Steps
Understanding Cyclobenzaprine’s place in recovery opens doors to explore broader topics such as enhanced recovery after surgery (ERAS), the role of regional anesthesia, and emerging non‑opioid analgesics. Readers interested in the pharmacology of muscle relaxants may also want to compare tizanidine or explore the impact of gabapentinoids on postoperative pain.
Frequently Asked Questions
Can I take Cyclobenzaprine with my home pain pills?
Yes, but only under a doctor’s guidance. The drug can interact with opioids, increasing sedation, and with SSRIs, raising serotonin syndrome risk. Adjust doses accordingly.
How soon after surgery should I start taking Cyclobenzaprine?
Usually within the first 24hours, once the patient is fully awake and can swallow tablets. Early use helps control spasm before it becomes entrenched.
What are the most common side effects I should watch for?
Dry mouth, mild dizziness, and drowsiness are the most frequent. If you notice heart rhythm changes, severe dizziness, or visual disturbances, contact your care team right away.
Is Cyclobenzaprine safe for older adults?
Older patients may be more sensitive to sedation and anticholinergic effects. Start at the lowest dose (5mg) and monitor closely for falls or confusion.
Can I stop Cyclobenzaprine abruptly after a week?
Short‑term use (under 2weeks) can usually be stopped without tapering. For longer courses, a gradual reduction helps avoid rebound spasm.


Peter Stephen .O 23.09.2025
This is the kind of post that makes me wanna high five the author. Cyclobenzaprine is basically the silent hero after surgery - no one talks about it but it’s the reason I could actually roll over in bed without screaming. Took it after my knee op and it was like my muscles finally got the memo to chill the hell out.
Also love how it’s not a magic bullet but a bridge. Pair it with PT and ibuprofen and boom - you’re walking again before you think you will.
Andrew Cairney 23.09.2025
They say it's for spasms but I bet Big Pharma just wanted another way to keep you hooked. 18 hour half life? That's not medicine, that's a slow drip of sedation. And why is it always 'moderate sedation'? That's just corporate speak for 'you'll nap through your kid's recital'.
Rob Goldstein 23.09.2025
As a PT who's seen this play out a hundred times - cyclobenzaprine is a game changer when used right. The key is timing. Start it within 24 hours, keep the dose low, and pair it with active recovery. It doesn't kill pain, it kills the guarding reflex that makes pain worse.
Patients who get it early? They’re out of the walker 3-5 days sooner. The real win isn't the drug - it's the momentum it gives rehab.
vinod mali 23.09.2025
Used this after my back surgery in Delhi. Doctor said 5mg thrice but I took only twice cause felt too sleepy. Worked fine. No drama. Just helped me move without feeling like my spine was glued shut.
Jennie Zhu 23.09.2025
It is imperative to underscore the pharmacokinetic rationale underpinning the three-times-daily dosing regimen. The 18-hour half-life, while ostensibly supporting TID administration, may result in subtherapeutic trough concentrations in patients with elevated metabolic clearance. A pharmacogenomic assessment of CYP3A4 activity is recommended prior to initiation.
Kathy Grant 23.09.2025
There’s something deeply human about how our bodies react to trauma - the way muscles clench like fists around a wound. Cyclobenzaprine doesn’t just relax muscles. It gives the nervous system permission to stop screaming. To stop fighting itself.
I’ve watched patients cry when they realized they could bend over to tie their shoes again. Not because the pain was gone - but because the fear was gone. And that? That’s medicine too.
Robert Merril 23.09.2025
Dude this drug makes you feel like a zombie but its the only thing that lets me move after surgery. I took it with oxycodone and just laid there for 3 days like a wet sack of potatoes but at least my back stopped feeling like it was being stapled shut. Also typo on the table says 5-10mg TID but I think they meant 5-10mg TID lol
Noel Molina Mattinez 23.09.2025
Why is no one talking about how this stuff is just a gateway to benzos? You take it for two weeks then you can't sleep without it then you start asking your doc for Xanax then next thing you know you're on a full cocktail. I've seen it. It's not a bridge. It's a trap door.
Roberta Colombin 23.09.2025
I appreciate how clear this is for patients. Many of us in recovery feel overwhelmed by medical jargon. This post helps people understand not just what the drug does, but why it matters - and how to use it safely. Thank you for writing with care.
Dave Feland 23.09.2025
The table is misleading. It compares cyclobenzaprine to methocarbamol and carisoprodol - two drugs that are largely obsolete in modern practice. The real comparison should be with tizanidine or baclofen, which have superior safety profiles and less anticholinergic burden. This post reads like a rep’s script from 2012.
Ashley Unknown 23.09.2025
I took this after my C-section and it made me feel like I was underwater. Like my thoughts were cotton and my limbs were lead. I started seeing things - shadows moving in the corner. My husband said I was talking nonsense. The nurse said it was just the meds. But I know what I saw. They’re hiding something. Why is this drug so widely prescribed if it makes people hallucinate? Why isn’t the FDA investigating? I’ve filed a report. They’re coming for us all.
Georgia Green 23.09.2025
Used this after my hip replacement. Took 5mg at 8am, 2pm, and 5pm. Felt a little dizzy but nothing crazy. My doc said not to take it after 6 but I did once at 7 and slept like a rock. Didn't regret it. Just... make sure you're not mixing it with anything else. My cousin had a bad reaction with her antidepressant. Don't be her.