H1 vs H2 Blocker Symptom Checker
Find the Right Medication for You
This tool helps you determine if you need an H1 blocker for allergies or an H2 blocker for stomach acid based on your symptoms. Remember: H1 blockers treat allergies, while H2 blockers treat stomach acid issues. Never mix them without medical advice.
Your Symptoms
Your Recommended Medication
Most people know antihistamines for stopping sneezing and itchy eyes, but not everyone realizes there are two completely different types: H1 and H2 blockers. They sound similar, but they work in totally different parts of your body and treat different problems. Mixing them up can lead to wasted money, unwanted side effects, or even dangerous mistakes. If you’re taking one of these and wondering why it’s not working-or why you’re feeling weird-you need to know which one you’re actually using.
What H1 Blockers Do and Who Uses Them
H1 blockers are the classic allergy pills you see on pharmacy shelves: Claritin, Zyrtec, Allegra, and Benadryl. They block histamine from binding to H1 receptors, which are found in your skin, nose, lungs, and blood vessels. That’s why they work so well for runny noses, hives, and itchy skin. These are the go-to for seasonal allergies, insect bites, and chronic urticaria.
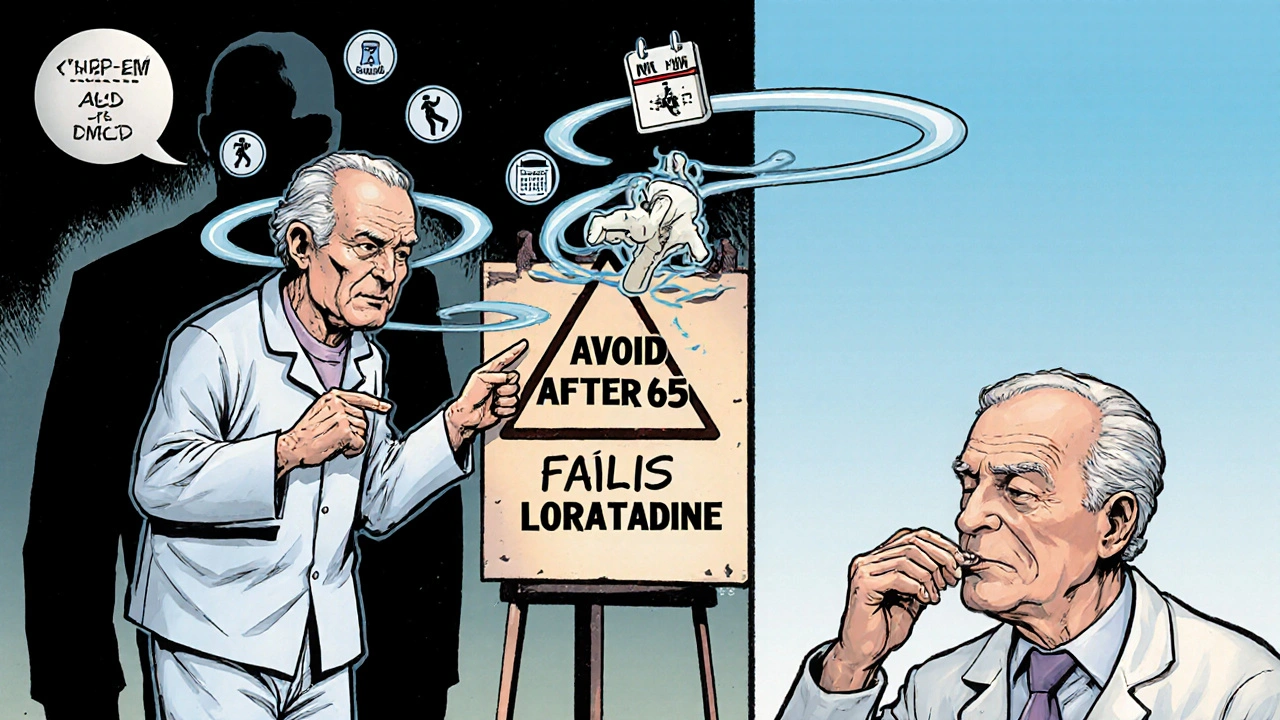
There are three generations of H1 blockers. First-gen, like diphenhydramine (Benadryl), cross the blood-brain barrier easily. That’s why they make you sleepy-up to half of users feel drowsy. That’s not a bug; it’s a feature for some. People take Benadryl at night to help sleep, even though it’s not approved for that. But if you’re driving, working, or caring for kids, this drowsiness is a real risk. Studies show first-gen antihistamines increase fall risk by 25-50% in older adults. The American Geriatrics Society specifically warns against them for people over 65.
Second- and third-gen options like loratadine and fexofenadine barely enter the brain. They cause drowsiness in only 10-15% of users. That’s why they’re the standard for daily use. They last 24 hours, so you take one pill a day. They’re also safer for long-term use and don’t interfere with memory like older versions do.
Side effects? Dry mouth is common-about 1 in 4 users. Blurred vision and trouble urinating happen less often, but they’re more likely with first-gen drugs. The FDA has also flagged some H1 blockers for rare but serious heart rhythm issues (QT prolongation) at high doses, especially with existing heart conditions or when mixed with other meds.
What H2 Blockers Do and Who Uses Them
H2 blockers are not for allergies. They’re for stomach acid. Drugs like famotidine (Pepcid) and cimetidine (Tagamet) block H2 receptors in your stomach lining. These receptors tell your stomach to pump out acid. Block them, and acid production drops-by 70% or more. That’s why they help with heartburn, GERD, and ulcers.
They kick in faster than proton pump inhibitors (PPIs), usually within 30-60 minutes. That’s why people take them before a big meal or spicy food. Effects last 10-12 hours. Many users report good relief, especially those who can’t tolerate PPIs due to long-term risks like nutrient deficiencies or gut bacteria changes.
But H2 blockers aren’t perfect. Side effects include headache (1 in 8 users), dizziness, and digestive issues like constipation or diarrhea. Cimetidine is especially tricky-it interferes with how your liver processes other drugs. It can affect blood thinners, seizure meds, and even some antidepressants. That’s why doctors avoid it now unless absolutely necessary. Famotidine is safer in that regard.
Remember Zantac? Ranitidine, an H2 blocker, was pulled from the market in 2020 because it was found to contain NDMA, a probable cancer-causing chemical. That shook consumer trust. Since then, famotidine has become the most common H2 blocker in the U.S. Still, some users report that the medicine stops working after weeks of daily use. That’s called tachyphylaxis-your body gets used to it. If your heartburn comes back stronger, it might be time to switch or add something else.
Side Effects Compared: H1 vs H2
It’s easy to think all antihistamines cause the same side effects. They don’t. Here’s how they really stack up:
| Side Effect | H1 Blockers (First-Gen) | H1 Blockers (Second-Gen) | H2 Blockers |
|---|---|---|---|
| Drowsiness | 30-50% | 10-15% | 5-8% |
| Dry Mouth | 25% | 15-20% | 5% |
| Blurred Vision | 15% | 5% | 1% |
| Headache | 5% | 5% | 12% |
| Constipation/Diarrhea | 5-10% | 3-5% | 10-15% |
| Urinary Retention | 5-10% | 1-2% | 1% |
| Drug Interactions | Low | Low | High (cimetidine only) |
First-gen H1 blockers are the worst offenders for anticholinergic effects-dry mouth, blurry vision, constipation, urinary retention. These are more than annoying. In older adults, they can trigger confusion, delirium, or falls. Second-gen H1 blockers are much cleaner. H2 blockers don’t cause these issues, but they bring their own: headaches and GI upset. And cimetidine? It’s a drug interaction nightmare. If you’re on more than a few medications, ask your doctor if famotidine is a better fit.
When to Use H1 vs H2 Blockers
Here’s the simple rule: H1 blockers for allergies. H2 blockers for acid.
If you’re sneezing, your eyes are watering, or you broke out in hives after eating shellfish-grab an H1 blocker. For daily allergy control, choose loratadine, cetirizine, or fexofenadine. Avoid diphenhydramine unless you’re using it as a sleep aid-and even then, only occasionally.
If you’re burning after meals, feeling bloated, or have chronic heartburn, H2 blockers are a good option. Famotidine works fast and is safe for short-term use. It’s also used before surgery to reduce stomach acid and prevent aspiration. But if you need daily relief for months, PPIs are stronger. H2 blockers can lose their punch over time.
There are rare cases where both are used together. For example, in mast cell activation syndrome or severe allergic reactions with stomach symptoms, some doctors combine them. Research is also looking into using H1 and H2 blockers together for heart failure, since histamine affects both blood vessels and heart muscle. But this is still experimental. Don’t mix them without medical advice.
What Users Really Say
Real-world experience tells a clear story. On Reddit’s r/Allergies, 68% of over 1,200 users said they switched from Benadryl to Claritin or Zyrtec because they didn’t want to feel drugged all day. Many said they kept Benadryl only for emergencies or nighttime use.
For H2 blockers, reviews on WebMD show most people get relief from heartburn-but about 30% say it doesn’t last. One user wrote: “Pepcid helps, but if I eat pizza, I’m back to square one in two hours.” Another said their dad, 72, got confused after taking cimetidine for a week. His doctor switched him to famotidine, and the fog lifted.
Success stories exist too. A 2022 case study in the Journal of Clinical Medicine described a woman with chronic hives who tried five different H1 blockers before bilastine cleared her symptoms completely. Another patient with GERD couldn’t take PPIs due to kidney issues-famotidine gave him stable relief for two years.
What You Should Avoid
Don’t use first-gen H1 blockers like Benadryl for daily allergies. The risks outweigh the benefits, especially if you’re over 65. The American Geriatrics Society says it plainly: avoid them.
Don’t use cimetidine unless your doctor specifically recommends it. There are safer H2 blockers available. Don’t take H2 blockers with alcohol-it increases dizziness and stomach upset.
Don’t assume all antihistamines are the same. Just because one makes you sleepy doesn’t mean the next one will. And never use an H2 blocker for an allergic reaction. It won’t help with swelling or breathing problems. Epinephrine is the only first-line treatment for anaphylaxis.
Final Takeaways
H1 and H2 blockers are not interchangeable. They’re two different tools for two different jobs. H1 blockers calm your body’s allergic response. H2 blockers quiet your stomach’s acid production. Confusing them can mean you’re treating the wrong thing-or making yourself sicker.
For allergies: Use second-gen H1 blockers like loratadine or fexofenadine. They’re safe, effective, and non-sedating. Keep first-gen versions like diphenhydramine for occasional use only.
For acid reflux: Famotidine is your best bet. It’s effective, widely available, and has fewer drug interactions than older H2 blockers. If it stops working, talk to your doctor about PPIs or other options.
If you’re on multiple medications, check for interactions. Especially if you’re taking cimetidine. And if you’re over 65, skip first-gen antihistamines entirely. There are better choices.
Know what you’re taking. Know why you’re taking it. And if you’re unsure, ask your pharmacist. They see these mix-ups every day.
Can I take H1 and H2 blockers together?
Yes, but only under medical supervision. Most people don’t need both. H1 blockers treat allergies; H2 blockers treat stomach acid. Combining them is rare and usually reserved for complex cases like mast cell disorders or severe allergic reactions with GI symptoms. Never combine them on your own.
Which is better for sleep: H1 or H2 blockers?
First-generation H1 blockers like diphenhydramine are commonly used for sleep because they cause drowsiness. H2 blockers don’t have this effect. But using H1 blockers regularly for sleep is not recommended-they can disrupt sleep quality over time and increase fall risk in older adults. Better sleep aids exist.
Are H2 blockers safe for long-term use?
Famotidine is generally safe for long-term use, especially compared to proton pump inhibitors (PPIs), which can cause nutrient deficiencies and gut issues with prolonged use. H2 blockers like famotidine have fewer long-term risks, though tolerance can develop. If you need daily acid control for months, talk to your doctor about whether H2 blockers are still the right choice for you.
Why was Zantac taken off the market?
Ranitidine (Zantac), an H2 blocker, was removed from the market in 2020 after the FDA found it contained NDMA, a chemical linked to cancer. The contamination worsened over time and with heat exposure. Famotidine (Pepcid) and nizatidine remain available and are not associated with this risk.
Can H1 blockers affect the heart?
Yes. Some H1 blockers, especially at high doses or in people with existing heart conditions, can cause QT prolongation-a heart rhythm issue that can lead to dangerous arrhythmias. This risk is rare but real. The FDA has issued warnings about certain antihistamines. Always tell your doctor about heart problems before taking any new medication.
What’s the best H1 blocker for allergies?
For most people, second-generation options like loratadine (Claritin), fexofenadine (Allegra), or cetirizine (Zyrtec) are best. They work for 24 hours, cause little to no drowsiness, and have minimal drug interactions. Bilastine is newer and even less sedating, but not yet widely available everywhere. Start with one of the first three.


Brierly Davis 6.11.2025
Man, I used to take Benadryl like candy before bed until I woke up feeling like a zombie and nearly knocked over my cat. Switched to Zyrtec and my sleep actually improved. No more midday crashes. Best decision ever.
Amber O'Sullivan 6.11.2025
Why do people still use cimetidine like its 1995 I swear some of you are living in a time capsule famotidine exists for a reason
Jim Oliver 6.11.2025
First-gen H1 blockers? You're not 'helping' your sleep-you're poisoning your brain with anticholinergics. And no, Pepcid won't cure your pizza-induced heartburn. You're just delaying the inevitable. Stop self-medicating.
William Priest 6.11.2025
bro i just took some zantac last week and i was fine?? why is everyone panicking? also i think h2 blockers are for allergies too?? wait no that's h1?? idk lol
Ryan Masuga 6.11.2025
Just wanted to say-this post saved me. I was taking Claritin for acid reflux because I didn’t know the difference. Thought they were all just 'allergy pills.' My stomach’s been calm for two weeks now. Thanks for breaking it down so simply. You’re a real one.
Jennifer Bedrosian 6.11.2025
I tried famotidine and it worked for like 3 days then BAM back to burning worse than before and I was like okay this is it I'm done with meds and just drink apple cider vinegar now and I feel like a wellness guru
Lashonda Rene 6.11.2025
So I’ve been on loratadine for like five years now for my seasonal allergies and honestly I didn’t even realize there were different kinds of antihistamines until I read this. I thought they were all the same. I used to take Benadryl back in college because it made me sleepy and I thought that meant it was stronger but now I know it was just making me dumber. I feel like I’ve been living in a fog for a decade. I’m switching to fexofenadine next refill. Also I think people over 65 should definitely avoid the old stuff because my grandma took diphenhydramine and she started forgetting where she was and talking to the TV and it was scary
Key Davis 6.11.2025
Thank you for this comprehensive overview. As a healthcare professional, I frequently encounter patients who conflate H1 and H2 blockers, often with serious consequences. The distinction is not merely academic-it is clinical. I encourage all readers to consult their pharmacist before combining medications or altering regimens. The data presented here aligns with current clinical guidelines, and the table comparing side effects is particularly valuable. Let us prioritize evidence over anecdote, and safety over convenience.