Nocturnal Urine Production Estimator
Understand Your Bed-Wetting Risk
This calculator estimates your nighttime urine production based on kidney function factors discussed in the article. Understanding your individual risk can help you make targeted adjustments to reduce bed-wetting episodes.
Important: This tool provides an estimate based on factors discussed in the article. Results are not medical advice. Consult a healthcare professional for personalized assessment and treatment.
Ever wonder why some kids (or adults) still wet the bed at night? It isn’t always a behavioral issue - the kidneys play a big part. Understanding how these organs manage fluid, hormones and nighttime urine can clear up confusion and point you toward practical fixes.
What are the kidneys?
Kidneys are a pair of bean‑shaped organs located near the lower back. They filter blood, remove waste, balance electrolytes, and regulate the volume of urine produced. Each kidney contains around a million nephrons, the tiny filtering units that turn blood into filtrate, which later becomes urine.
How the kidneys control urine production
The amount of urine you make isn’t constant; it shifts with hydration, activity, and hormones. Two key players are:
- Antidiuretic hormone (ADH) - released by the pituitary gland, ADH tells the kidneys to re‑absorb water, making urine more concentrated.
- Renin‑angiotensin‑aldosterone system (RAAS) - adjusts sodium and water balance, influencing how much fluid stays in the bloodstream.
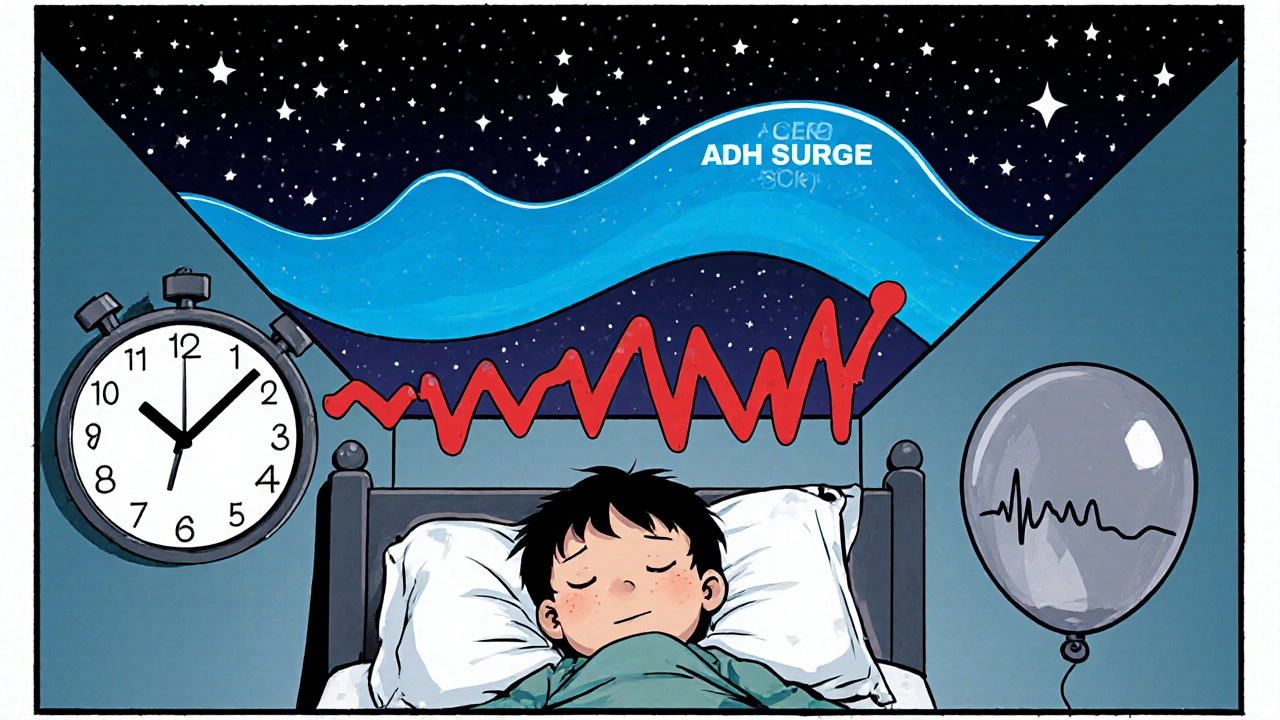
During the day, when you’re moving and drinking, ADH levels dip, so the kidneys dump excess fluid. At night, ADH should rise, signaling the kidneys to conserve water and produce less urine. If this surge is blunted, you’ll wake up with a full bladder and possibly wet the bed.
The night‑time balance: circadian rhythm and ADH
Our internal clock (circadian rhythm) orchestrates hormone release. Around 10p.m., ADH peaks, reducing urine output. However, several factors can disrupt this rhythm:
- Stress or anxiety - spikes cortisol, which can suppress ADH.
- Late‑night fluid intake - overwhelms the kidneys before ADH fully kicks in.
- Sleep disorders such as obstructive sleep apnea - cause intermittent hypoxia, altering hormone patterns.
When ADH doesn’t rise enough, the kidneys continue to filter fluid at a daytime rate, filling the bladder faster than the body can wake up.
When kidney function directly contributes to bed-wetting
Several kidney‑related scenarios increase nocturnal urine volume:
- Reduced ADH production - common in children under four, who haven’t fully matured their pituitary response.
- Chronic kidney disease (CKD) - impairs the kidneys’ ability to concentrate urine, leading to higher output.
- Diabetes mellitus - high blood sugar forces the kidneys to excrete excess glucose, pulling water along (osmotic diuresis).
- Medication side effects - diuretics, lithium, or certain antihypertensives increase urine volume.
In each case, the bladder fills faster than the body’s alarm system, creating a classic bed‑wetting episode.
Medical conditions that link kidneys to bed-wetting
Beyond kidney disease, other health issues can indirectly affect kidney‑controlled urine production:
| Condition | How it Impacts Kidneys | Typical Bed‑Wetting Pattern |
|---|---|---|
| Type1 Diabetes | Osmotic diuresis from high glucose | Frequent, high‑volume nighttime wetting |
| Sleep Apnea | Intermittent hypoxia reduces ADH release | Sudden, occasional episodes after a bad night |
| Urinary Tract Infection (UTI) | Inflammation irritates bladder, increases urgency | Urgent wetting with possible pain |
| Congenital Kidney Anomalies | Reduced concentrating ability from birth | Persistent bed-wetting despite behavioral training |
Identifying the pattern helps clinicians decide whether to focus on the kidneys, the bladder, or an external factor.
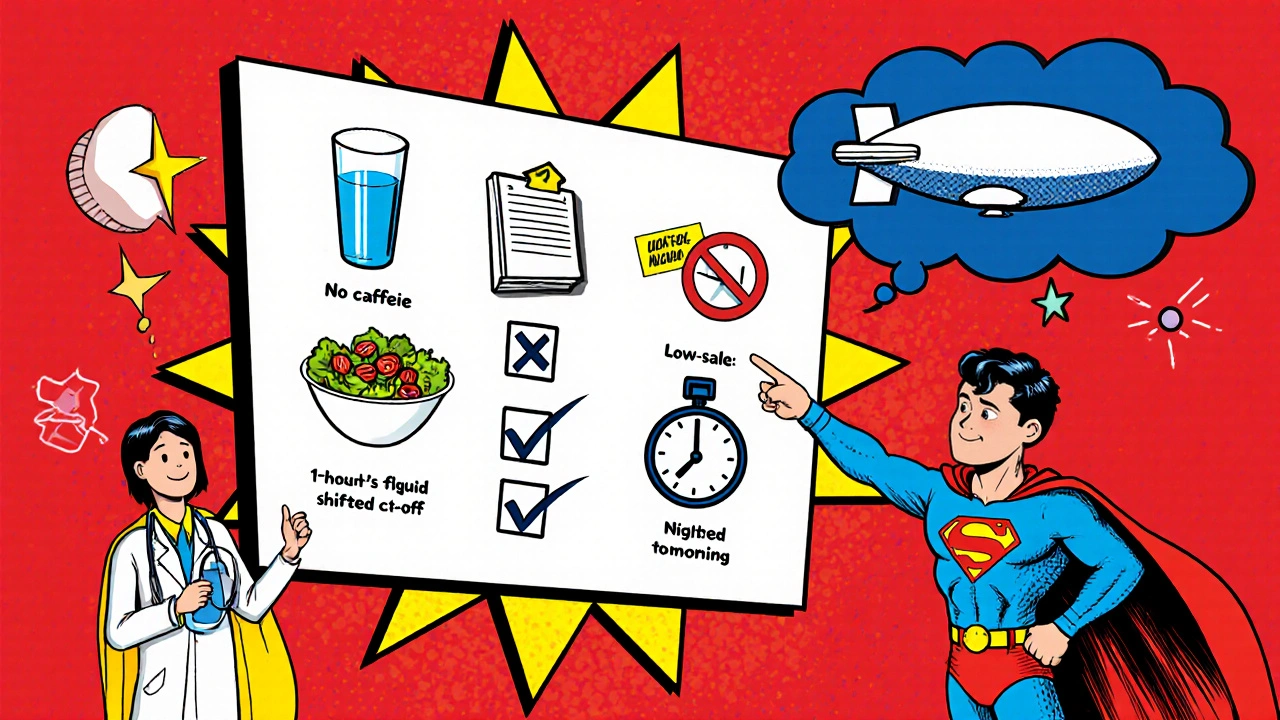
Practical steps to manage kidney‑related bed‑wetting
These actions target fluid balance, hormone regulation, and bladder health:
- Limit fluids after dinner - aim for a 1‑2hour window before bedtime.
- Choose water over caffeine or sugary drinks - caffeine can blunt ADH, while sugar adds extra osmotic load.
- Schedule a bathroom trip right before sleep - empties the bladder and reduces nighttime pressure.
- Monitor urine color - pale yellow suggests adequate hydration; dark urine may indicate dehydration, prompting the kidneys to conserve water.
- Consider a low‑salt diet - excess sodium forces the kidneys to excrete more water.
- Check medication timing - move diuretics to earlier in the day if possible.
- Track night‑time incidents - a simple diary helps spot trends (e.g., wetting after a weekend of high fluid intake).
When these adjustments don’t help, it’s time to talk to a healthcare professional.
When to see a doctor
Seek medical advice if you notice any of these red flags:
- Bed‑wetting persists beyond age7 (for children) or suddenly starts in adulthood.
- Accompanying symptoms such as pain, frequent urges, or fever.
- Signs of diabetes: increased thirst, unexplained weight loss.
- History of kidney problems or a family history of CKD.
- Use of medications known to affect urine output.
A doctor may order blood tests (creatinine, glucose), urine analysis, or a sleep study to pinpoint the underlying cause.
Quick checklist for parents and adults
- Limit evening fluids - especially caffeine and sugary drinks.
- Use the bathroom right before bed.
- Observe urine color and volume.
- Keep a wet‑night diary for at least two weeks.
- Review medication schedules with a pharmacist.
- Consult a doctor if episodes continue after a month of adjustments.
Frequently Asked Questions
Why do some children outgrow bed‑wetting while others don’t?
Most kids develop a stronger ADH surge and better bladder capacity by age5‑6. Persistent cases often involve a slower hormonal maturation, underlying kidney issues, or genetic factors that keep the ADH response low.
Can drinking water earlier in the day reduce night‑time wetting?
Yes. Spreading fluid intake across the day gives the kidneys time to process the volume while ADH is naturally lower, leaving less fluid to be dealt with during the night.
Is a low‑salt diet really effective for bed‑wetting?
Reducing sodium cuts down on the water the kidneys need to excrete to keep blood balance, which can lower overall urine volume at night. It’s a simple dietary tweak that often helps.
Do diuretics cause bed‑wetting in adults?
They can. Diuretics increase urine production, especially if taken late in the day. Switching the dose to the morning or adjusting the type can alleviate nighttime episodes.
When should a sleep study be considered?
If the person snorts loudly, pauses breathing, or experiences daytime fatigue alongside bed‑wetting, a sleep apnea work‑up is warranted because the condition directly disrupts ADH release.


Pranesh Kuppusamy 16.10.2025
The renal system orchestrates fluid balance with a precision that borders on the metaphysical. By filtering blood each minute the kidneys generate a milieu that informs hormonal release. At night antidiuretic hormone should ascend, yet subtle disruptions can invert this rhythm. When such a surge is muted, the bladder fills as if it were daytime, leading to nocturnal enuresis. This cascade underscores how a hidden physiological agenda may be at work in many cases.
Crystal McLellan 16.10.2025
they dont tell you that big pharma is pushing diuretics to keep us all in a constant state of dependence its a silent agenda that messes with our nighttime hormones and makes bed‑wetting a side effect of their profit scheme
Kelly Thomas 16.10.2025
Think of your kidneys as the night‑shift custodians of your body’s water balance – they sweep away excess fluid while your brain’s ADH alarm clock whispers “hold on”. If that whisper is too soft, the night‑time urine output spikes and the bladder can’t hold the flood. Simple tricks like a fluid‑free window before bed, a low‑salt dinner, and a bathroom pit‑stop can tip the scales back in your favor. Consistent monitoring of urine colour gives you a visual cue: pale yellow means you’re on track, dark amber warns of dehydration and over‑compensation. By treating the kidneys as partners rather than obstacles, many families see a dramatic drop in wet‑night incidents within weeks.
Alison Poteracke 16.10.2025
While it’s easy to jump to grand conspiracies, the practical steps outlined in the article-like limiting evening fluids and timing diuretics-address the issue without invoking hidden agendas.
Marianne Wilson 16.10.2025
It’s a misstep to blame kidneys alone; attributing enuresis solely to renal function oversimplifies a multifactorial problem and neglects the psychosocial dimensions that truly shape nocturnal habits.
Patricia Bokern 16.10.2025
OMG the night‑time wetting saga is like a horror movie where the kidneys are the secret villains sneaking in under the moonlight and dumping pee everywhere! I swear the whole thing feels like a plot twist nobody warned us about.
Garrett Gonzales 16.10.2025
The pathophysiology involves a dysregulated hypotonic state mediated by reduced arginine‑vasopressin secretion, leading to increased glomerular filtration rate and nocturnal polyuria. Adjusting the pharmacokinetics of antihypertensive agents can mitigate this effect.
Aman Deep 16.10.2025
The kidney is not merely a pair of bean‑shaped filters but a nocturnal sentinel that watches over the tide of our inner waters. When the circadian clock whispers its midnight hymn, antidiuretic hormone should rise like a quiet tide, urging the nephrons to conserve every drop. Yet in many of us that signal is a faint murmur, and the kidneys continue their daytime hustle, spilling fluid into the bladder. This mismatch creates a perfect storm where the bladder fills faster than the brain’s arousal system can react. Imagine a city that keeps its sprinklers on at 3 a.m.; the streets will flood and the residents will wake drenched. The same principle applies to our internal plumbing, and the result is a wet sheet that tells a story of hormonal discord. Factors like stress, late‑night caffeine, or even hidden sleep‑apnea can sabotage the ADH surge, turning night into a leaky faucet. Moreover, conditions such as early‑stage chronic kidney disease or uncontrolled diabetes act like cracked reservoirs, letting more water escape. The good news is that lifestyle tweaks-like a two‑hour fluid curfew, a low‑salt dinner, and a bedtime bathroom routine-act as dam builders. Monitoring urine colour provides a visual dashboard: a pale shade signals balance, while a dark hue warns of dehydration‑induced over‑compensation. If these interventions fail, a targeted medical work‑up can reveal whether the ADH axis or renal concentrating ability is at fault. Simple lab tests-serum osmolality, creatinine, and a fasting glucose-often expose hidden culprits. In some cases, adjusting diuretic timing or swapping to a different antihypertensive class restores the night‑time equilibrium. And remember, a supportive bedtime ritual-perhaps a calming story or soft music-can lower cortisol, indirectly protecting ADH release. So, by respecting the kidney’s night‑shift duty and harmonizing our habits, we can turn those midnight drizzles into dry, peaceful slumbers 😊🌙.
Nicola Gilmour 16.10.2025
Thank you for the thorough breakdown; the analogies really help visualize the process and make the recommendations feel achievable.
Darci Gonzalez 16.10.2025
You’ve got this! 🌟