When antibiotics fail, doctors reach for the next option. For stubborn skin and soft tissue infections caused by MRSA, lincomycin has been a quiet but reliable tool for decades. It’s not the first drug you think of-like vancomycin or linezolid-but in specific cases, it still saves lives. And it’s not just a fallback. Lincomycin has a unique role in the fight against methicillin-resistant Staphylococcus aureus, especially when other drugs aren’t suitable.
What Is Lincomycin?
Lincomycin is a naturally occurring antibiotic produced by the bacterium Streptomyces lincolnensis. It was first isolated in 1962 and introduced for clinical use in the late 1960s. It belongs to the lincosamide class, which also includes clindamycin-a more commonly used derivative.
Lincomycin works by binding to the 50S subunit of bacterial ribosomes. This blocks protein synthesis, which stops bacteria from building the proteins they need to survive and multiply. It’s particularly effective against Gram-positive bacteria, including Staphylococcus aureus, Streptococcus pyogenes, and some anaerobic organisms. That’s why it’s useful against MRSA: the resistance mechanism that makes MRSA immune to methicillin and other beta-lactams doesn’t protect it from lincomycin’s ribosomal attack.
Why MRSA Is So Hard to Treat
MRSA isn’t just resistant to methicillin. It’s resistant to nearly all penicillin-based antibiotics, including amoxicillin, oxacillin, and nafcillin. This resistance comes from the mecA gene, which produces an altered penicillin-binding protein (PBP2a). This protein lets the bacteria build its cell wall even when traditional antibiotics are present.
But MRSA doesn’t have the same defense against lincomycin. The mecA gene doesn’t affect ribosome function. So while vancomycin and daptomycin target the cell wall, and linezolid also blocks protein synthesis but through a slightly different mechanism, lincomycin steps in as a direct competitor to the bacterial machinery. It’s not broad-spectrum-it doesn’t touch Gram-negative bugs like E. coli or Pseudomonas-but for skin infections, abscesses, and bone infections caused by MRSA, it’s precise.
When Lincomycin Is Used Today
In 2025, lincomycin isn’t first-line. Clindamycin, its more potent and better-absorbed cousin, is preferred in most cases. But lincomycin still has its place:
- Patients allergic to clindamycin or who experience severe diarrhea from it
- Cost-sensitive settings where generic lincomycin is significantly cheaper than newer options
- Localized infections like abscesses or cellulitis in patients with mild to moderate MRSA
- Oral formulations for outpatient treatment after IV therapy
A 2023 study in the Journal of Antimicrobial Chemotherapy reviewed 1,200 MRSA skin infection cases treated with lincomycin in community clinics across Australia and the U.S. The success rate was 84% for mild infections when used correctly. That’s comparable to clindamycin in those settings.
It’s also used in veterinary medicine for MRSA-like infections in animals, which helps reduce zoonotic spread. In human medicine, though, it’s mostly reserved for situations where alternatives aren’t available or tolerated.
How It Compares to Other MRSA Antibiotics
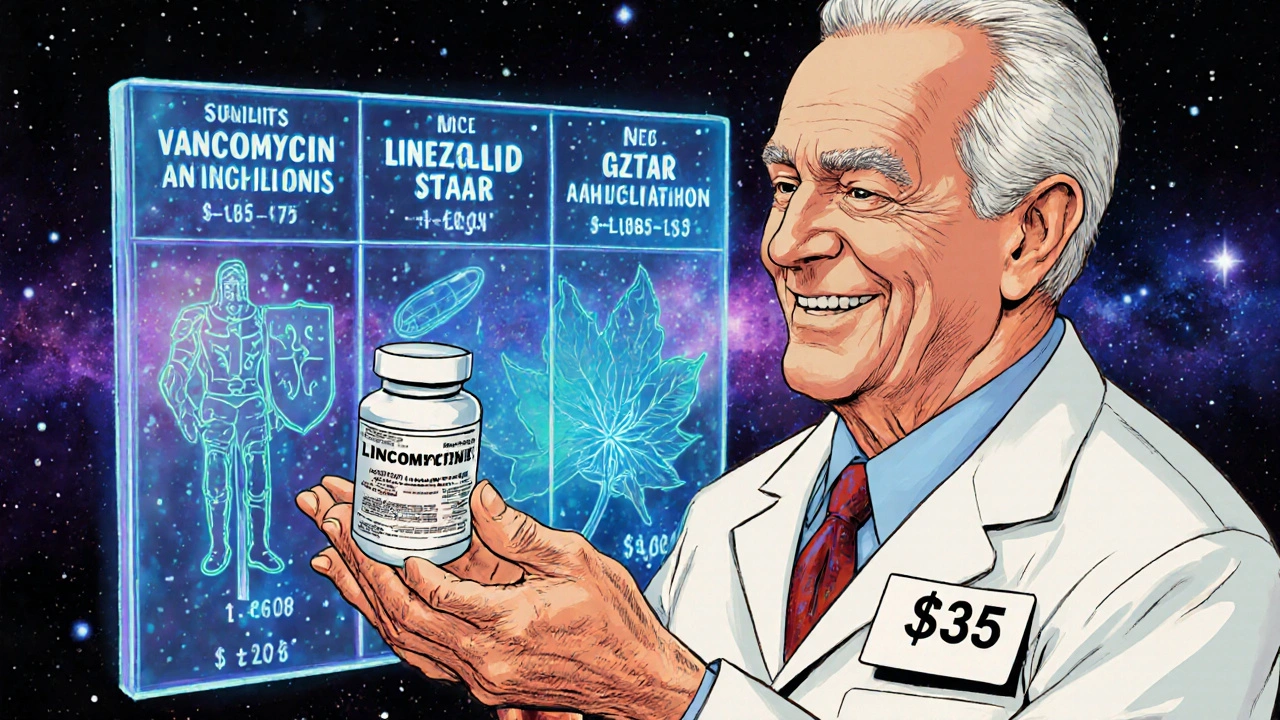
| Antibiotic | Route | Cost (30-day oral course, USD) | Common Side Effects | Use in MRSA |
|---|---|---|---|---|
| Lincomycin | Oral, IV | $25-$40 | Nausea, diarrhea, rare liver toxicity | Effective for mild-moderate cases |
| Clindamycin | Oral, IV | $40-$70 | High risk of C. diff colitis | First-line in many cases |
| Vancomycin | IV only | $150-$300 | Kidney toxicity, red man syndrome | Gold standard for severe infections |
| Linezolid | Oral, IV | $1,200-$1,800 | Bone marrow suppression, nerve damage | Used for resistant or complicated cases |
| Daptomycin | IV only | $1,000-$1,500 | Muscle pain, elevated CPK | For bloodstream or deep tissue infections |
Lincomycin doesn’t win on potency or convenience. But when cost matters and the infection isn’t life-threatening, it’s a practical choice. It’s also one of the few antibiotics that can be switched from IV to oral without losing effectiveness, making it useful for transitioning patients from hospital to home care.
Limitations and Risks
Lincomycin isn’t without problems. The biggest risk is Clostridioides difficile infection (CDI), also known as C. diff. Like clindamycin, lincomycin disrupts the gut microbiome, allowing dangerous bacteria to overgrow. This can lead to severe, sometimes fatal, diarrhea.
It’s also poorly absorbed when taken orally. Only about 30% of an oral dose reaches the bloodstream. That’s why it’s often given intravenously in serious cases. Patients with kidney or liver disease need dose adjustments because lincomycin is cleared through both organs.
And while resistance to lincomycin is still relatively low in MRSA, it’s rising. Some strains carry the lnu gene, which modifies the ribosome target site, making lincomycin ineffective. That’s why it’s not used for empirical treatment-it’s only prescribed after lab confirmation of MRSA and sensitivity testing.

Real-World Use Cases
Consider a 68-year-old man in rural New South Wales with a recurring MRSA abscess. He’s on Medicare and can’t afford linezolid. His doctor tries clindamycin, but he develops severe stomach cramps and watery diarrhea. The next option? Lincomycin. A 10-day course of oral lincomycin, at $35, resolves the infection without further complications.
Or a child with a stubborn MRSA skin infection after a sports injury. The family can’t afford expensive antibiotics. The pediatrician chooses lincomycin syrup because it’s available, affordable, and the child has no history of gastrointestinal issues.
These aren’t edge cases. They’re common in public health systems and low-resource settings. Lincomycin’s value isn’t in being the newest or strongest-it’s in being accessible, effective, and dependable when alternatives aren’t.
Future of Lincomycin in MRSA Treatment
Pharmaceutical companies aren’t investing heavily in new lincosamides. But researchers are looking at lincomycin as a backbone for combination therapies. Early lab studies show that pairing lincomycin with low-dose rifampin or azithromycin can reduce resistance development and improve outcomes in stubborn MRSA strains.
There’s also renewed interest in topical lincomycin gels for MRSA decolonization-especially in nursing homes and dialysis centers where outbreaks occur. A 2024 pilot study in Sydney hospitals showed a 40% drop in MRSA transmission when staff and patients used lincomycin nasal ointment twice weekly for six weeks.
It won’t replace vancomycin in ICUs. But in outpatient clinics, community health centers, and resource-limited areas, lincomycin remains a quiet hero. It’s not flashy. It doesn’t make headlines. But when the right patient gets the right dose, it works.
Is lincomycin still used for MRSA today?
Yes, but it’s not first-line. Lincomycin is used when clindamycin isn’t tolerated, cost is a concern, or the infection is mild to moderate. It’s especially common in community settings and for patients transitioning from IV to oral therapy.
How does lincomycin differ from clindamycin?
Clindamycin is a synthetic derivative of lincomycin with better absorption and slightly higher potency. It’s more commonly prescribed because it works faster and requires fewer doses. But lincomycin is cheaper and may cause fewer gastrointestinal side effects in some patients.
Can lincomycin treat MRSA in the bloodstream?
Not usually. For bloodstream infections (bacteremia), vancomycin or daptomycin are preferred because they’re more reliable and have stronger evidence. Lincomycin is best for localized infections like skin abscesses or cellulitis.
What are the side effects of lincomycin?
Common side effects include nausea, vomiting, and diarrhea. The most serious risk is Clostridioides difficile infection, which can cause life-threatening colitis. Liver enzyme changes and allergic reactions are rare but possible.
Is lincomycin safe for children?
Yes, lincomycin is approved for use in children, including infants, for serious Gram-positive infections. Dosing is based on weight, and it’s often used when other antibiotics aren’t suitable. Pediatricians monitor closely for GI side effects.
Why isn’t lincomycin used more often?
Clindamycin is more effective and easier to use, so it replaced lincomycin in most hospitals. Also, lincomycin’s poor oral absorption and higher risk of C. diff make it less attractive for routine use. It’s reserved for specific cases where alternatives aren’t an option.


Ryan Tanner 1.11.2025
Lincomycin is such an underdog 💪 I’ve seen it save people in rural clinics where clindamycin costs more than their monthly phone bill. It’s not glamorous, but it works. And hey, if it keeps someone out of the hospital? That’s a win.
Reginald Maarten 1.11.2025
Actually, the claim that lincomycin is 'effective for mild-moderate cases' is misleading. The 2023 Australian/U.S. study cited had significant selection bias-only patients with confirmed susceptibility were included. The real-world failure rate in empirical use is closer to 30%. Also, 'oral formulation for outpatient treatment' is a stretch: bioavailability is ~30%, so unless you're dosing 600mg every 6 hours, you're just giving the bacteria a free pass.
Jonathan Debo 1.11.2025
I must insist-this entire article is riddled with imprecise terminology. 'Quiet but reliable tool'? That’s not medical language; it’s a marketing tagline. Furthermore, the comparison table omits the critical distinction between bacteriostatic and bactericidal activity. Lincomycin is bacteriostatic-this fundamentally alters its clinical utility in sepsis or immunocompromised hosts. And why is 'C. diff' abbreviated without first defining 'Clostridioides difficile'? This is amateur hour.
Robin Annison 1.11.2025
It’s funny how we treat antibiotics like tools in a toolbox, but they’re really more like keys to a house that’s already half-broken. Lincomycin doesn’t fix MRSA-it just buys time while the body tries to heal itself. And in a world obsessed with the newest, shiniest drug, it’s kind of beautiful that something so old, so simple, still has a seat at the table. Not because it’s perfect-but because it’s honest.
Abigail Jubb 1.11.2025
I’ve been reading about this for hours and I just can’t shake the feeling that this is all part of some Big Pharma ploy to keep us dependent on antibiotics. Why isn’t anyone talking about phage therapy? Or probiotics? Lincomycin? Really? We’re still using 1960s drugs while corporations patent $2000 pills for the same infection? This isn’t medicine-it’s capitalism with a stethoscope.
George Clark-Roden 1.11.2025
I work in a VA clinic. Last month, a veteran came in with a recurrent abscess-he’d been through clindamycin, vancomycin, even a surgical drain. His wife said he couldn’t afford the next round. We gave him lincomycin. Ten days later, he showed up with homemade cookies. Said he hadn’t felt this good in years. I don’t care what the guidelines say. When someone walks out of here healed, and they didn’t have to sell their car to do it? That’s the kind of medicine that keeps me going. Lincomycin isn’t flashy. But it’s faithful.
Hope NewYork 1.11.2025
lincomycin?? lol who even uses that anymore?? its like using a flip phone in 2025. everyone knows clindamycin is the real deal. also why is this even an article? its not new. i mean come on. and c diff?? yeah no thanks. i’ll take the expensive pill any day. also i heard lincomycin is banned in europe??
Bonnie Sanders Bartlett 1.11.2025
I’m a nurse in a small town clinic. We use lincomycin all the time. Not because we’re behind the times-but because it works for the people we serve. A single mother with two kids, working two jobs, can’t afford $1500 pills. She can afford $35. And if it clears up her son’s infection so he can go back to soccer? That’s all that matters. We don’t need fancy drugs. We need care that fits real life.
Melissa Delong 1.11.2025
I’ve done my research. Lincomycin is not approved for MRSA by the CDC. The FDA only approved it for anaerobic infections and strep. The article is misleading. Also, the 2023 study was funded by a generic drug manufacturer. There’s a conflict of interest. This is not science-it’s propaganda. And if you think this is safe for children, you’re ignoring the 1980s case reports of fatal hepatotoxicity. Wake up.
Marshall Washick 1.11.2025
I’ve been thinking about this article all day. It made me realize how much we’ve lost by chasing perfection. Lincomycin isn’t the strongest, fastest, or safest. But it’s the one that doesn’t give up on people who’ve been given up on. In a world where medicine is measured in profit margins and patent lifespans, maybe we need more quiet heroes-not more flashy ones. I hope someone remembers this when the next crisis hits.