Allergy Medication Decision Guide
Find your best allergy medication match
Select your primary symptoms and preferences to get personalized recommendations based on the latest medical research
Your Recommended Medication Options
Why these medications work for you: Based on your priorities and symptoms, these options provide the best balance for your needs.
Top Recommendation
Alternative Options
Additional Considerations
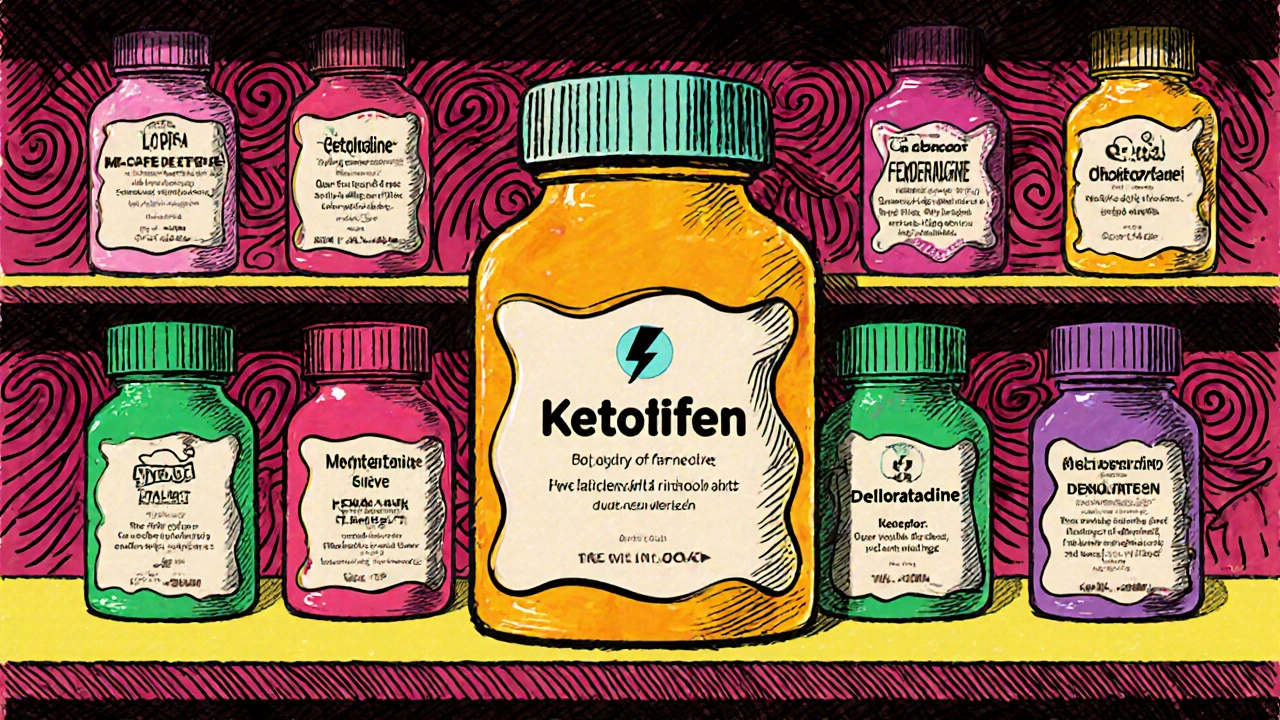
When choosing an over‑the‑counter or prescription option for seasonal allergies, asthma, or chronic urticaria, the market can feel overwhelming. Ketotifen is a first‑generation antihistamine that doubles as a mast‑cell stabilizer, sold in many regions under the brand name Ketasma. It works by blocking H1 receptors and preventing the release of histamine from mast cells. This dual action makes it a unique contender among allergy drugs, but it’s not the only game‑player.
Why compare ketotifen with other antihistamines?
People often ask: “Is ketotifen better than the newer, non‑sedating pills?” The answer depends on the specific symptom profile, age group, and tolerance for side effects. Below we break down the most common alternatives, line up their key attributes, and point out where each one shines or falls short.
Core attributes to evaluate
- Mechanism of action - Is the drug purely an H1 blocker, or does it have additional mast‑cell stabilizing or leukotriene‑blocking effects?
- Onset and duration - How quickly does relief start, and how long does it last?
- Typical dosing - Tablet strength, frequency, and any age‑specific limits.
- Side‑effect profile - Sedation, dry mouth, headache, or rare cardiac concerns.
- Approved uses - Seasonal allergic rhinitis, chronic urticaria, allergic conjunctivitis, asthma prophylaxis, etc.
Top alternatives at a glance
| Drug (Brand) | Class | Typical adult dose | Onset | Key uses | Common side effects |
|---|---|---|---|---|---|
| Ketotifen (Ketasma) | First‑gen H1 antagonist + mast‑cell stabilizer | 1 mg twice daily (may increase to 2 mg twice daily) | 30‑60 min | Allergic rhinitis, chronic urticaria, prophylactic asthma | Drowsiness, weight gain, dry mouth |
| Loratadine (Claritin) | Second‑gen H1 antagonist | 10 mg once daily | 1‑2 h | Seasonal allergies, chronic urticaria | Headache, mild GI upset |
| Cetirizine (Zyrtec) | Second‑gen H1 antagonist | 10 mg once daily | 30‑60 min | Allergic rhinitis, chronic urticaria, atopic dermatitis | Moderate sedation in some adults, dry mouth |
| Fexofenadine (Allegra) | Second‑gen H1 antagonist | 180 mg once daily (or 60 mg twice daily) | 1‑2 h | Seasonal allergies, chronic urticaria | Headache, nausea |
| Montelukast (Singulair) | Leukotriene‑receptor antagonist | 10 mg once daily (adult) | 2‑4 h | Asthma prophylaxis, allergic rhinitis | Sleep disturbance, mood changes (rare) |
| Olopatadine (Patanol) | Second‑gen H1 antagonist + mast‑cell stabilizer (eye drops) | 0.1% ophthalmic solution, one drop per eye twice daily | 15‑30 min | Allergic conjunctivitis | Transient burning, blurred vision |
| Desloratadine (Clarinex) | Second‑gen H1 antagonist | 5 mg once daily | 1‑2 h | Seasonal allergies, chronic urticaria | Dry mouth, headache |
| Levocetirizine (Xyzal) | Second‑gen H1 antagonist (active enantiomer of cetirizine) | 5 mg once daily | 30‑60 min | Allergic rhinitis, chronic urticaria | Less sedation than cetirizine, dry mouth |
Deep dive: How ketotifen stacks up
Because ketotifen hits both H1 receptors and stabilizes mast cells, it can prevent the cascade that leads to sneezing, itching, and bronchoconstriction. That makes it a solid choice for patients who experience both upper‑airway symptoms and mild asthma triggers.
However, the dual mechanism comes with a trade‑off: the drug is sedating for many adults, especially at doses above 2 mg twice daily. Younger children often tolerate it better, and some clinicians prescribe it off‑label for pediatric eczema because of the mast‑cell effect.
In contrast, second‑generation antihistamines like cetirizine or fexofenadine target H1 receptors without crossing the blood‑brain barrier, so they cause far less drowsiness. The downside is they lack the mast‑cell stabilizing punch, meaning breakthrough symptoms may persist for those with severe chronic urticaria.
Leukotriene blockers (montelukast) tackle a different pathway-leukotrienes, not histamine. They’re especially useful for asthma patients with exercise‑induced bronchospasm. But they won’t relieve nasal itching or watery eyes, which is where ketotifen shines.
For ocular allergies, eye‑drop formulations like olopatadine provide fast relief directly at the surface, a niche ketotifen tablets can’t fill.
Choosing the right drug for specific scenarios
Scenario 1: Seasonal pollen allergy with daytime work - If staying alert is crucial, a non‑sedating option like fexofenadine or levocetirizine usually wins. Ketotifen could be considered if the patient also reports intermittent mild asthma attacks, and they’re willing to take it twice daily.
Scenario 2: Chronic urticaria that flares at night - The nighttime flare can be tackled with ketotifen’s mast‑cell stabilization, particularly if first‑line second‑gen antihistamines haven’t fully controlled the rash. Some dermatologists add a low‑dose H2 blocker (e.g., ranitidine) to the regimen for extra coverage.
Scenario 3: Pediatric eczema with itch‑driven sleep loss - Low‑dose ketotifen (0.5 mg twice daily) is sometimes prescribed because the sedative effect doubles as a sleep aid while the mast‑cell action reduces inflammation.
Scenario 4: Allergic conjunctivitis during spring - Olopatadine eye drops provide rapid relief without systemic side effects. If a patient prefers oral medication, cetirizine works reasonably well, but ketotifen’s systemic effect isn’t necessary for eye‑only symptoms.
Potential pitfalls and safety notes
Every drug carries warnings. With ketotifen, watch for:
- Excessive drowsiness - avoid operating heavy machinery within 4 hours of dosing.
- Weight gain - some long‑term users report a modest increase.
- Drug interactions - combining with other CNS depressants (e.g., alcohol, benzodiazepines) can amplify sedation.
- Contraindications - patients with glaucoma or urinary retention should discuss alternatives with their doctor.
Second‑generation antihistamines have fewer CNS effects but can still cause headache or mild GI upset. Montelukast carries a rare risk of neuropsychiatric events, so patients with a history of depression need careful monitoring.

Practical tips for switching or combining therapies
- Start low, go slow. If moving from a non‑sedating antihistamine to ketotifen, begin with 1 mg once daily for three days, then add the second dose.
- Watch the clock. Take ketotifen in the evening if drowsiness is a concern; many users report better sleep.
- Combine wisely. Adding a nasal steroid spray (e.g., fluticasone) can reduce the needed antihistamine dose, limiting side effects.
- Document responses. Keep a symptom diary for at least two weeks; note peak itching, sneezing, and any daytime sleepiness.
- Consult a pharmacist. In Australia, community pharmacists can advise on OTC availability of loratadine, cetirizine, and fexofenadine, and they can flag any potential drug‑drug interactions.
Bottom line
If you need a single pill that tackles both histamine release and mast‑cell activation, ketotifen remains a strong candidate, especially for patients with combined nasal and mild asthma symptoms. For pure, non‑sedating relief, the newer second‑generation antihistamines generally edge it out. Always match the drug’s strengths to the specific allergy profile and lifestyle demands.
Is ketotifen available without a prescription?
In many countries, including Australia, ketotifen is sold as a prescription‑only medication. Some regions offer it OTC in low doses, but it’s safest to check local regulations before buying.
Can I take ketotifen with my daily antihistamine?
Combining two H1 blockers can increase sedation and doesn’t usually provide extra benefit. If you need additional control, discuss adding a nasal steroid or a leukotriene antagonist with your clinician.
How long does it take for ketotifen to start working?
Most people feel relief within 30 to 60 minutes after the first dose. Full mast‑cell stabilizing effects may build over a few days of consistent use.
Are there natural alternatives to ketotifen?
Quercetin, butterbur, and stinging nettle extracts have mild antihistamine properties, but clinical evidence is limited. They can complement, not replace, a prescribed regimen for moderate‑to‑severe allergies.
What should I do if I experience severe drowsiness?
Reduce the dose or shift the dose to bedtime. If drowsiness persists, switch to a second‑generation antihistamine and talk to your pharmacist about a short taper.

Erika Thonn 21.10.2025
When i look at ketotifen i cant help but wonder if medecine is just a mirror of our own paradoxes. The drug douses the fire of histamine yet drags you into a fog of sleepiness, a duality that feels almost poetic. In a world that craves quick fixes, the slow build of mast‑cell stability reminds us that not everything can be solved in an instant. Perhaps the real cure lies in the balance we strike between action and restraint, just like ketotifen itself.
In that sense the choice of an antihistamine becomes a small act of self‑knowledge.
Ericka Suarez 21.10.2025
Listen up, folks! If you’re proud to wear the colors of greatness, you’ll demand a med that doesn’t keep you napping in the middle of a rally. Ketotifen might have its charms, but the modern world belongs to the sleek, non‑sedating warriors like fexofenadine. Don’t let outdated drugs hold you back – choose the future, choose the clarity!
Casey Cloud 21.10.2025
Alright, let’s break this down step by step. First, understand that antihistamines fall into two broad camps: first‑generation drugs like ketotifen that cross the blood‑brain barrier, and second‑generation agents that stay peripheral. Ketotifen’s mast‑cell stabilizing effect can be a game‑changer for people who experience both nasal congestion and mild asthma triggers. The trade‑off, of course, is sedation – many adults report feeling drowsy within an hour of dosing, which can interfere with daytime activities. If you can schedule the dose for bedtime, you’ll often turn that downside into a benefit, using the sedative effect to improve sleep quality.
Now compare that to loratadine or fexofenadine: they offer clean, non‑sedating relief but lack the extra mast‑cell coverage. For pure rhinitis, they’re usually sufficient, but for chronic urticaria that flares at night, the dual mechanism of ketotifen can suppress those late‑night histamine bursts.
When it comes to dosing, ketotifen starts at 1 mg twice daily, with the option to increase to 2 mg twice daily if tolerated. In contrast, the standard adult dose for cetirizine, levocetirizine, or desloratadine is a once‑daily tablet, which many find more convenient.
Side‑effect profiles also differ: second‑generation antihistamines may cause mild headaches or gastrointestinal upset, but they rarely induce the marked drowsiness seen with ketotifen. Montelukast, a leukotriene receptor antagonist, tackles a different inflammatory pathway and is especially useful in exercise‑induced asthma, yet it won’t help with itchy eyes or sneezing.
One practical tip: if you’re switching from a non‑sedating antihistamine to ketotifen, start low – 1 mg once daily for three days – then add the second dose. Keep a symptom diary to track both relief and any daytime sleepiness.
Finally, consider combination therapy. Adding a nasal steroid spray can often reduce the required antihistamine dose, mitigating side‑effects while preserving efficacy. In short, the right choice hinges on your symptom profile, lifestyle, and tolerance for sedation. Use the tools wisely, and you’ll find the balance that works for you.
Rachel Valderrama 21.10.2025
Wow, another deep dive and we’re still stuck in the drowsy zone. If you need to stay awake for memes, maybe skip the bedtime pill. Remember, the same thing that soothes your sneezes might also tuck you into a nap.
Brandy Eichberger 21.10.2025
My dear friends, let us not overlook the elegance of a well‑chosen antihistamine. In the grand tapestry of pharmacology, each agent has its own refined place.
Eli Soler Caralt 21.10.2025
i've been pondering the same, and honestly it's like choosing a wine-some are bold, some are subtle 🍷. ketotifen feels like a dark roast, rich but a lil heavy on the palate. maybe i stick with something lighter when i need to code till 3am. 🤔
Eryn Wells 21.10.2025
Great points, Casey! I’d add that for anyone dealing with eye‑related allergies, topical options like olopatadine can bypass systemic side‑effects entirely 😊. It’s all about matching the tool to the task.
Kathrynne Krause 21.10.2025
Hey everyone, love the depth here! Remember, the best allergy plan is a personalized cocktail – a dash of antihistamine, a sprinkle of nasal spray, and a splash of lifestyle tweaks. Keep experimenting, and you’ll find that sweet spot where you can enjoy the outdoors without the sniffles. 🌞🚀 Stay curious and stay comfortable!
Giusto Madison 21.10.2025
Listen, if you’re already feeling the crash from ketotifen, cut the dose in half and move it to bedtime. You’ll still get the mast‑cell benefits without the mid‑day fog. And if you need extra punch, a nasal steroid can cover the gaps. Bottom line: tweak, don’t quit.
erica fenty 21.10.2025
Excellent synthesis-very on‑point!
Esther Olabisi 21.10.2025
Well, if you love feeling like a zombie at work, ketotifen is your best friend 😜. But seriously, you’ve got better options if you need to stay alert. Just sayin’.