When your doctor switches your antidepressant or antipsychotic, it’s not just a change in pills. For many, it feels like losing a part of yourself. You might not realize it until you’re two weeks in, staring at the mirror, wondering why you feel numb, anxious, or like you’re floating outside your body. This isn’t just side effects. It’s a psychological earthquake.
The Hidden Psychological Cost of Switching
Most people assume switching medications is a simple swap-take one off, start another. But the mind doesn’t work that way. A 2023 study from King’s College London tracked over 40,000 people on antidepressants. Nearly 1 in 9 switched within 90 days. Why? Because the first drug didn’t work. Or because insurance forced a change. Or because a pharmacist substituted a generic without telling them. The psychological fallout? It’s real. One participant in a 2016 NIH study, referred to as Bart, saw his avoidance behaviors drop from over five responses per minute to just over one after his quetiapine dose was lowered. That’s not just a chemical change-it’s a behavioral collapse. People report feeling like strangers in their own skin. One Reddit user wrote: “I lost six months of progress. I didn’t recognize myself.” The American Psychiatric Association formally recognized this in DSM-5, calling out medication discontinuation syndromes. These aren’t just physical tremors or dizziness. They’re emotional unraveling: sudden panic, rage, suicidal thoughts, or a crushing sense of betrayal. And it’s not rare. A 2022 NAMI survey found 63% of people experienced psychological distress during a switch. Over a third reported suicidal ideation.Why Generics Can Feel Like a Betrayal
The biggest trigger? Switching from a brand-name drug to a generic-or worse, switching between different generics. Patients don’t know it’s happening. A pharmacist fills the prescription. The pill looks different. The size, color, or filler ingredients change. And suddenly, the stability they fought for over months crumbles. A 2019 review by Dr. Pierre Blier found that 68% of problematic switches happened between different generic versions of the same drug-not between brand and generic. That’s critical. It’s not about cost. It’s about the act of switching itself. Your brain adapts to a specific formulation. Even tiny differences in how the drug is absorbed can destabilize someone who’s barely holding on. One patient on PatientsLikeMe switched from brand-name sertraline to a generic and experienced complete emotional numbness for three weeks, followed by panic attacks that hadn’t hit in two years. She ended up hospitalized. Her doctors didn’t connect the dots. Neither did the pharmacist. The system didn’t warn anyone.How Your Brain Reacts to Change
Psychiatrists now describe three psychological phases people go through when changing meds:- Loss of self-This happens early. You’ve been on the drug long enough that it’s become part of your identity. You don’t remember what “normal” felt like before. When you stop, you feel like you’re disappearing.
- Chaotic adaptation-This is the worst part. Electric-shock sensations in the head. Dizziness. Insomnia. Emotional volatility. One in four people describe feeling like a junkie begging for their old pill. It’s not addiction. It’s neurochemical recalibration. But your brain doesn’t know that.
- Stable acceptance-Only 35% of people reach this stage after two years. The rest are still cycling, switching, or stuck in limbo.

Who Gets Left Behind
This isn’t equal. People with lower incomes are 33% more likely to have negative psychological outcomes during a switch. Why? They’re more likely to be switched without consent-because insurance denies coverage. They’re less likely to have the time or resources to see a specialist. They’re more likely to be on multiple meds, making the switch even more dangerous. University-educated patients are 25% less likely to switch antidepressants. That’s not because they’re healthier. It’s because they know to ask questions. They push back. They demand explanations. They track their symptoms. Most people don’t have that privilege. And primary care doctors? They’re managing 85% of mental health prescriptions now. But only 22% of family medicine residencies teach proper switching protocols. Many don’t know how long to taper paroxetine (21-hour half-life) versus fluoxetine (96-hour half-life). One wrong taper can send someone into crisis.What Works-And What Doesn’t
Cross-tapering-gradually reducing the old drug while slowly introducing the new one-is the gold standard. It cuts psychological side effects by 37% compared to quitting cold turkey. But it takes time. Two to four weeks. Weekly check-ins. Patient education. Most systems don’t support it. Electronic health records? Only 37% have built-in switching protocols. Doctors often don’t document the switch clearly. Patients get confused. They stop taking the new drug because they think it’s not working. Or they go back to the old one because they feel better. Then they’re back in the cycle. The FDA’s 2022 draft guidance finally acknowledged that bioequivalence doesn’t equal therapeutic equivalence for CNS drugs. That’s huge. But it’s still just guidance. No enforcement. No mandatory testing. Digital tools are helping. Pear Therapeutics’ reSET app, cleared by the FDA in 2023, tracks mood, sleep, and adherence during switches. In a trial of 1,200 patients, it reduced hospitalizations by 27%. But it’s not widely available. Most people still rely on their doctor’s memory-and their own notes.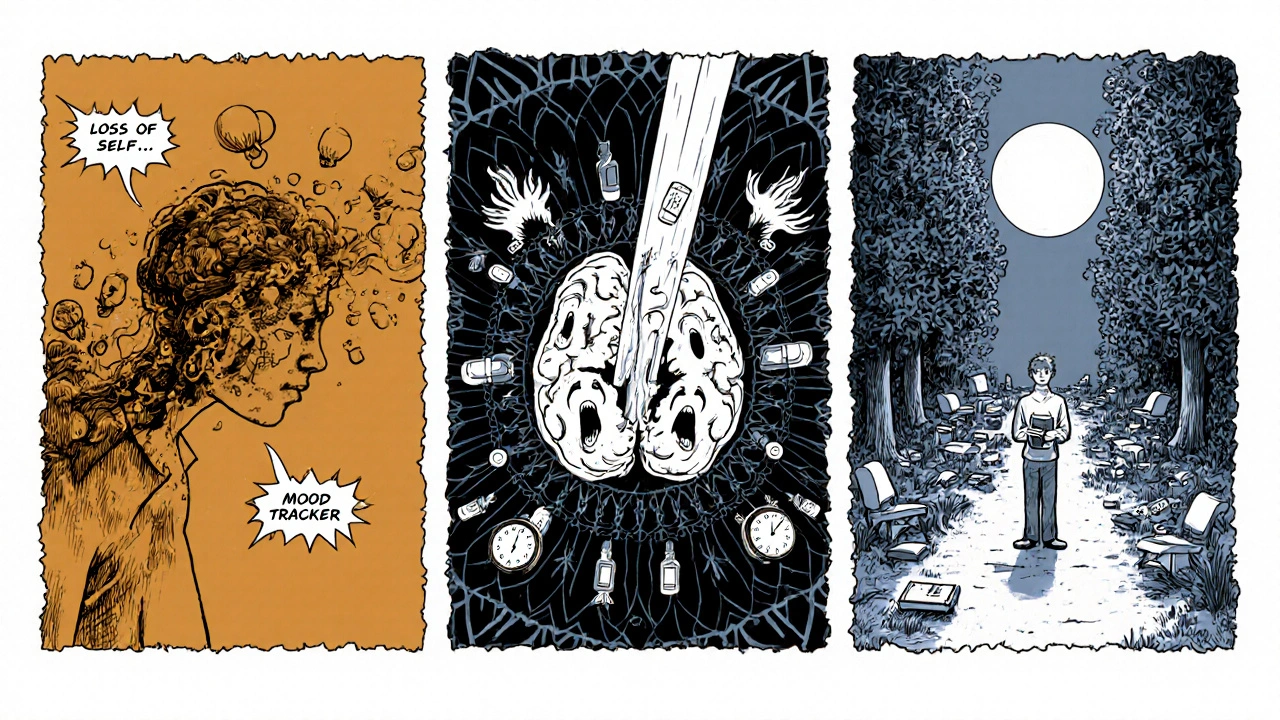
What to Do If You’re Being Switched
If your doctor says you’re switching:- Ask: Why now? Is it because the drug isn’t working-or because your insurance won’t cover it?
- Ask: What’s the plan? Will it be a cross-taper? How long? What symptoms should I watch for?
- Ask: Is this a brand or a generic? If it’s generic, which manufacturer? Ask for the name on the bottle. Keep a record.
- Track your mood, sleep, energy, and physical symptoms daily. Use a free app or a notebook. Bring it to every appointment.
- Insist on a follow-up within one week. Don’t wait until your next scheduled visit.
- If you feel worse-don’t wait. Call your doctor. Go to urgent care. This isn’t normal.
The Bigger Picture
Medication switching isn’t just a medical issue. It’s a trust issue. When patients are switched without warning, they feel abandoned. They stop believing in their treatment. One Psych Central poll found 74% of users felt less confident in their care after an unplanned switch. We treat mental illness like a broken pipe-just turn the valve, replace the part. But the mind isn’t a machine. It’s a fragile, adaptive system. Changing the chemical input doesn’t just change the output-it changes how you see yourself, how you relate to others, how you feel about the future. The system is broken. But you’re not. If you’ve been switched and feel lost, you’re not crazy. You’re reacting to a process that wasn’t designed for you. It’s time we stop treating psychiatric medication changes like routine pharmacy transactions. They’re life-altering events. And they deserve more than a signature on a form.Can switching antidepressants cause depression to get worse?
Yes. Studies show that 71% of patients who were switched from branded to generic antidepressants without their knowledge experienced worsening symptoms or relapse. Even when the new drug is technically equivalent, the act of switching can destabilize the brain’s chemical balance, leading to increased anxiety, emotional numbness, or suicidal thoughts. This is especially common with medications that have short half-lives, like paroxetine or venlafaxine.
Why do I feel different after switching to a generic medication?
Generic medications must meet FDA standards for bioequivalence, but they can differ in fillers, binders, and how the drug is released in your body. These small differences can affect absorption, especially for drugs with narrow therapeutic windows like SSRIs and antipsychotics. Many patients report feeling “off,” emotionally flat, or anxious after switching-even when blood levels are identical. The psychological impact often comes from the disruption of a stable routine, not just chemistry.
How long does it take to adjust after switching psychiatric meds?
Adjustment time varies. For most antidepressants, it takes 2-6 weeks to feel stable on a new drug. But psychological symptoms like anxiety, dizziness, or emotional blunting can last longer-sometimes months. The NIH study found that behavioral changes continued for up to two years in some cases. A slow cross-taper (over 3-4 weeks) reduces the timeline and severity of symptoms. Rushing the process increases the risk of relapse or withdrawal.
Is it safe to switch medications without my doctor’s guidance?
No. Abruptly stopping or switching psychiatric medications can trigger severe withdrawal symptoms, including seizures, psychosis, or suicidal ideation. Even over-the-counter supplements can interfere. Always work with a prescriber who understands tapering schedules, pharmacokinetics, and your personal history. Self-switching is dangerous and often leads to hospitalization.
What should I ask my doctor before agreeing to a medication switch?
Ask: Why are we switching? Is this because the drug isn’t working, or is it due to cost or insurance? What’s the tapering plan? How long will it take? What symptoms should I watch for? Will I be switched to a brand or generic? Can I get the same manufacturer if it’s generic? When should I schedule my next check-in? Write these down. If your doctor can’t answer clearly, seek a second opinion.
Are there tests that can predict if I’ll react badly to a switch?
Pharmacogenetic tests can identify genetic variations that affect how you metabolize certain drugs. Companies like Genomind offer these, and they’re growing in use. But they’re not yet standard. Only 15% of primary care providers use them regularly. While they can help predict side effects or poor response, they can’t guarantee a smooth switch. They’re a tool-not a crystal ball.
Can switching meds cause long-term mental health damage?
In some cases, yes. Repeated switches, especially without proper tapering, can lead to kindling-a phenomenon where the brain becomes more sensitive to changes over time. This can make future switches harder and increase the risk of chronic anxiety, mood instability, or treatment-resistant depression. The longer you’re on a stable regimen, the more fragile that stability becomes. Avoid unnecessary switches.


Ryan Airey 14.11.2025
This is why I don't trust Big Pharma or the FDA. They don't care if you're emotionally shattered as long as the pill counts match on paper. That 68% stat? That's not a glitch-it's the system working exactly as designed. Generics aren't 'equivalent,' they're cost-cutting placeholders for people who can't afford to feel human.
Ogonna Igbo 14.11.2025
Look I'm from Nigeria and we don't even have access to these fancy brand name drugs most times but I've seen people go mad after switching from one generic to another. No one explains anything. You get a new bottle, you take it, then you're crying for no reason or laughing at nothing. Doctors say it's stress. It's not stress. It's the damn pill changing your soul without asking. We need laws here too. Not just in the US.
Aidan McCord-Amasis 14.11.2025
Bro I switched from Zoloft to generic sertraline and went full zombie for 3 weeks. Then panic attacks. Then cried in the shower for 45 minutes straight. I didn't even know I could feel that empty. 🤡
BABA SABKA 14.11.2025
Pharmacokinetics isn't a buzzword-it's survival. The difference between 1.2% and 1.8% bioavailability in a drug with a narrow therapeutic window isn't statistical noise, it's a neurochemical grenade. You're not 'imagining' the change. Your receptors are rewiring mid-flight while your insurance company saves $12 a month. That's not healthcare. That's corporate roulette.
Jonathan Dobey 14.11.2025
They call it 'bioequivalence' like it's a scientific fact. But the brain doesn't read lab reports. It reads rhythm. Consistency. The texture of your daily stability. When you swap a pill, even if the active ingredient is identical, you're breaking a sacred covenant your nervous system made with that specific molecular arrangement. It's not chemistry-it's betrayal encoded in cellulose and magnesium stearate.
John Foster 14.11.2025
There's a deeper metaphysical layer here. We treat the mind as a machine because we fear its mystery. But when you switch meds, you're not adjusting a setting-you're erasing a version of yourself that took years to build. The numbness isn't side effect. It's grief. Grief for the person you were before the pill became your armor. And nobody wants to admit that the real problem isn't the drug-it's that we've outsourced identity to a pharmacy.
Edward Ward 14.11.2025
Just to clarify: cross-tapering isn't just 'recommended'-it's the only ethical approach. The 37% reduction in psychological side effects? That's not a suggestion. That's a moral imperative. Yet, in primary care, patients are often told to 'stop one and start the other tomorrow.' That's not medical practice. That's negligence dressed in white coats. And the fact that only 37% of EHRs have built-in protocols? That's not an oversight. That's systemic dehumanization.
Jessica Chambers 14.11.2025
So let me get this straight… you’re telling me the system is designed so that people with less money are more likely to be switched without warning, less likely to understand what’s happening, and more likely to end up in the ER… and the solution is to ‘track your mood in a notebook’? 😂
ASHISH TURAN 14.11.2025
My cousin switched from brand to generic fluoxetine and started hearing voices. Not metaphorical. Actual voices. Told his mom the fridge was talking to him. Took 6 weeks to stabilize. No one connected it. He’s still on meds but now he won’t trust any pill unless it’s the exact same blue oval from the same pharmacy. It’s not paranoia. It’s survival.
Chris Bryan 14.11.2025
This is all part of the globalist agenda to depopulate the mentally ill. They don't want you stable. They want you broken so you'll take more drugs, pay more bills, and never question the system. The FDA? The AMA? All controlled by the same cabal that owns the pharmaceutical patents. Read the fine print on those generic labels. The fillers? They're laced with neurotoxins. You think it's coincidence that switches spike suicide rates? It's intentional.
Hollis Hollywood 14.11.2025
I’ve been on the same sertraline for 8 years. My therapist says I’m one of the few who didn’t need to switch. But I’ve watched friends go through this-some never come back. I used to think it was just ‘bad luck.’ Now I see it’s structural violence. People don’t get to choose their stability. Only the rich can afford to keep their minds intact. That’s the real tragedy here.
Shyamal Spadoni 14.11.2025
did u kno that the fda allows generics to vary by up to 20% in absorption? that means if ur drug is supposed to release 50mg over 12 hrs, it could release 60 or 40. for antipsychotics? that's like driving a car with brakes that work sometimes. and doctors dont even check blood levels. its a joke. i think they do it on purpose to keep us dependent.
Adam Dille 14.11.2025
My mom switched from Lexapro to generic escitalopram and became a different person. Didn't recognize her. Took 5 months to get back to baseline. She still says, 'I didn't feel like me until I got the old blue pill back.' I told her to save the bottle. Now she keeps it in a shoebox like a relic. We all need to do that. Keep the pill. Keep the name. Keep the fight.
Katie Baker 14.11.2025
Just wanted to say-this post saved me. I thought I was going crazy after switching. Turns out I’m not broken. The system is. You’re not alone. And you deserve better than a pharmacy shuffle.
Andrew Eppich 14.11.2025
While the emotional anecdotes are compelling, we must not conflate subjective experience with clinical evidence. Bioequivalence is a scientifically validated standard. If patients report adverse effects, it may be attributable to nocebo effects, poor adherence, or comorbid conditions-not the medication switch itself. To suggest otherwise undermines the integrity of pharmacological science.