When your nose runs, gets stuffy, or sneezes without any pollen or pet dander around, it’s not allergies. It’s nonallergic rhinitis. This condition affects up to 23% of adults in Western countries, and many people don’t even know they have it. They assume it’s a cold, or that they’re just sensitive to weather changes. But if symptoms last more than three months and allergy tests come back negative, you’re likely dealing with nonallergic rhinitis - a chronic condition driven by irritants, not immune reactions.
What Exactly Is Nonallergic Rhinitis?
Nonallergic rhinitis isn’t one disease. It’s a group of conditions that cause nasal symptoms like runny nose, congestion, and sneezing - but without the involvement of IgE antibodies, which define true allergies. Think of it like a faulty thermostat in your nose. Instead of responding to allergens, it overreacts to everyday triggers: cold air, strong smells, spicy food, or even changes in humidity. It’s not an infection. It’s not an allergy. It’s a nervous system glitch in the nasal lining. The most common subtype is vasomotor rhinitis, making up 60-70% of cases. Studies show this happens because the autonomic nerves controlling blood flow in the nose get out of balance. Too much parasympathetic activity means blood vessels swell, mucus glands go into overdrive, and you end up with a constant drip or blockage. Advanced imaging has found that TRPV1 receptors - the same ones that make chili peppers feel hot - are overexpressed in these patients. That’s why temperature shifts and chemical irritants hit so hard.The Top 6 Irritant Triggers You Can’t Ignore
Unlike allergic rhinitis, where triggers are mostly airborne allergens, nonallergic rhinitis reacts to a wide range of physical and chemical stimuli. Here are the six main categories, backed by clinical data:- Environmental irritants: Tobacco smoke (as little as 0.05 mg/m³), perfume (0.1 ppm), paint fumes (50 ppm VOCs), and wildfire smoke (15 µg/m³ PM2.5) can all set off symptoms. Even cleaning products or air fresheners can trigger a reaction.
- Weather changes: A drop or rise of just 5°C in temperature, or a humidity shift of over 20%, can cause nasal congestion. This is why people in Sydney often notice worse symptoms during seasonal transitions - especially in winter when indoor heating dries the air.
- Food and drink: Spicy foods with capsaicin (like hot peppers) trigger rhinorrhea in 55-60% of older adults. Alcohol, even at low blood levels (0.02%), can cause flushing and runny nose. Hot soups or curry aren’t just comforting - they’re potential triggers.
- Medications: Blood pressure drugs like ACE inhibitors (used by millions) cause symptoms in 20% of users. Beta-blockers affect 15%. NSAIDs like ibuprofen can worsen it in 10-15% of people. Hormone replacement therapy and birth control pills are also linked to flare-ups.
- Hormonal shifts: Pregnancy affects 20-30% of women, especially in the second trimester. Puberty and thyroid dysfunction also trigger episodes. This isn’t coincidence - it’s physiology.
- Occupational exposures: Flour dust (2 mg/m³), latex particles (2 µg/m³), and chemical vapors in factories or labs can lead to work-related rhinitis. Studies show symptoms worsen by 37% over the workweek in these cases.
How Doctors Diagnose It (And Why It’s Often Missed)
There’s no single test for nonallergic rhinitis. Diagnosis is all about ruling things out. First, your doctor will check for allergies using skin prick tests or blood tests for IgE. If those are negative - and symptoms last over three months - nonallergic rhinitis is likely. Nasal endoscopy may be used to rule out polyps or structural issues. A nasal smear showing neutrophils (not eosinophils) confirms the diagnosis. But here’s the problem: 30-40% of cases are misdiagnosed as allergic rhinitis. Patients end up on antihistamines that do nothing, or even undergo expensive allergy shots that won’t help. A 2023 study found that primary care doctors correctly identify nonallergic rhinitis in only 25-30% of cases. That’s why many people go years without proper treatment.Effective Management: What Actually Works
Treatment isn’t one-size-fits-all. The goal is to reduce triggers and calm the overactive nasal response. Here’s what works, based on clinical evidence:1. Trigger Avoidance - The First Line of Defense
Simple changes make a big difference. Using a HEPA filter reduces symptoms by 35-40%. Avoiding strong scents (perfumes, detergents, air fresheners) cuts flare-ups by 25-30%. For gustatory rhinitis, cutting out very spicy foods or hot drinks can reduce symptoms by 40-50%. If you work around dust or fumes, wearing a mask helps - especially in environments like bakeries or labs.2. Nasal Saline Irrigation - Simple, Safe, and Effective
Rinsing your nose with salt water (isotonic or hypertonic) is one of the most underused tools. It clears irritants, reduces inflammation, and improves mucus flow. Studies show 60-70% of users get relief. Twice-daily rinsing works better than once. Many users report improved sense of smell and fewer medication needs. A neti pot or squeeze bottle works fine - just use distilled or boiled water.3. Intranasal Corticosteroids - The Gold Standard for Moderate to Severe Cases
Fluticasone (Flonase) or mometasone (Nasonex) are first-line prescriptions. They reduce inflammation in the nasal lining, even though this isn’t a classic allergic inflammation. These sprays take 2-4 weeks to peak but can cut symptoms by 50-60%. Side effects? Minor nosebleeds occur in 15-20% of users - but they’re usually mild and improve with proper technique.4. Ipratropium Bromide - The Runny Nose Killer
This nasal spray (Atrovent) is the only treatment specifically designed for rhinorrhea. It blocks the nerves that signal mucus production. Within 48 hours, users often see an 70-80% drop in runny nose. It doesn’t help with congestion, but if your main problem is dripping, this is the most effective option. FDA trials show maximum effect at two weeks. A newer 0.03% formulation (approved in 2023) works just as well with fewer side effects.5. Azelastine Nasal Spray - A Middle Ground
Though developed for allergies, azelastine (Astelin) also helps nonallergic rhinitis. It reduces symptoms by 30-40% and works within 1-2 hours. But 30-40% of users report a bitter taste - which can be annoying. Still, for people who don’t respond to steroids or ipratropium, it’s a solid option.6. Avoid Decongestant Sprays - They Make It Worse
Nasal decongestant sprays (like oxymetazoline) give quick relief - but only for 3-5 days. After that, you get rebound congestion. This is called rhinitis medicamentosa, and it’s a vicious cycle. If you’ve been using these sprays for weeks or months, stopping cold turkey can make symptoms worse for 7-10 days. The fix? Switch to a nasal steroid during withdrawal. Studies show 85-90% of people recover fully with this approach.What Doesn’t Work - And Why
Oral antihistamines (like loratadine or cetirizine) are commonly prescribed - but they’re largely ineffective for nonallergic rhinitis. Why? Because they target histamine, which isn’t the main driver here. The same goes for allergen immunotherapy (allergy shots). If you’ve tried these without relief, it’s not your fault - it’s the wrong diagnosis.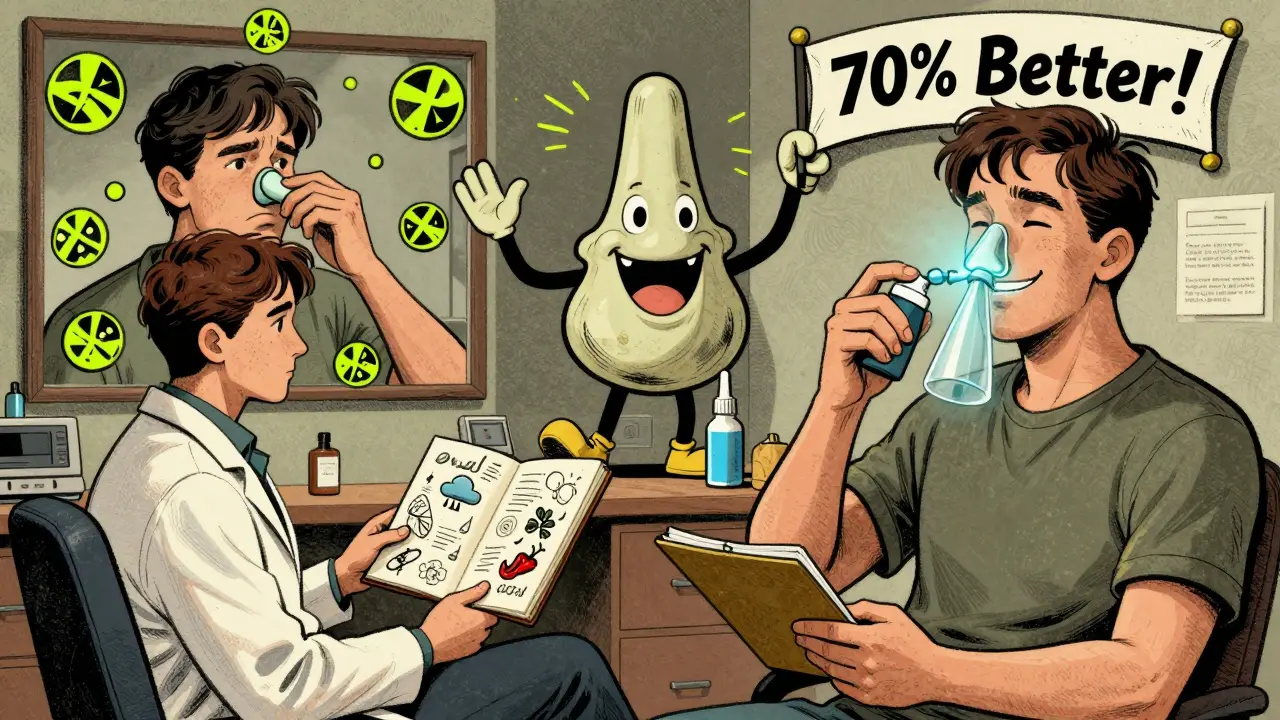
Real Patient Experiences
On patient forums, common stories emerge. One woman in Sydney said her runny nose started during pregnancy and never went away. She tried antihistamines for two years - nothing. Then she started saline rinses and ipratropium. Within a week, the dripping stopped. Another man, a chef, noticed his nose ran every time he cooked spicy dishes. He cut back on chili, started using a mask at work, and now only uses nasal spray when needed. But many still struggle. One Reddit user shared: “I’ve been told I’m allergic, then told I’m not. I’ve tried everything. No one gets it.” That’s why tracking your triggers matters. Keep a simple diary: note the date, temperature, humidity, what you ate, what you smelled, and how bad your nose felt. After 4-6 weeks, patterns emerge. You might realize your symptoms spike every time the AC turns on - or after coffee. That’s your personal trigger list.What’s Next? The Future of Treatment
Researchers are looking beyond symptom control. A new class of drugs called TRPV1 antagonists - which block the overactive heat-sensing receptors in the nose - is in phase 2 trials. Early results show 50-60% symptom reduction in tough cases. The FDA and EMA are reviewing these drugs, with potential approval by 2027. Other innovations include nasal neurostimulation devices. A small pilot study at Johns Hopkins used mild electrical pulses to calm overactive nerves - and saw a 45% drop in symptoms. These aren’t mainstream yet, but they point to a future where treatment targets the root cause, not just the symptoms.Final Thoughts: You’re Not Alone
Nonallergic rhinitis isn’t life-threatening, but it’s exhausting. Constant sniffles, blocked sinuses, and the frustration of being told “it’s just allergies” can wear you down. The good news? You don’t have to live with it. With the right diagnosis and a targeted plan - avoiding triggers, using saline, and choosing the right nasal spray - most people regain control. Start simple: get tested for allergies. If negative, try saline rinses twice a day. If that doesn’t help, talk to your doctor about ipratropium or a nasal steroid. Avoid decongestant sprays. Track your triggers. And know this: you’re not imagining it. Your nose isn’t broken - it’s just reacting to the world in a way that’s poorly understood. But now, you know how to manage it.Is nonallergic rhinitis the same as allergies?
No. Allergies involve the immune system and IgE antibodies reacting to specific triggers like pollen or pet dander. Nonallergic rhinitis is caused by irritation of the nasal lining from things like smoke, cold air, or spicy food - without any immune response. Allergy tests will come back negative if you have nonallergic rhinitis.
Can weather changes really trigger nasal symptoms?
Yes. Even small changes in temperature (over 5°C) or humidity (over 20%) can cause blood vessels in the nose to swell and mucus to increase. This is especially common during seasonal transitions or in air-conditioned environments. People in Sydney often notice worse symptoms in winter when indoor heating dries the air and causes rapid temperature shifts.
Why don’t antihistamines work for nonallergic rhinitis?
Antihistamines block histamine, a chemical released during allergic reactions. But in nonallergic rhinitis, histamine isn’t the main problem. The issue is nerve overactivity and blood vessel swelling. That’s why antihistamines often do nothing - they’re treating the wrong mechanism.
Is nasal saline irrigation really that helpful?
Yes. Studies show 60-70% of users get symptom relief. It washes out irritants, reduces inflammation, and improves mucus flow. Twice-daily rinsing is more effective than once. It’s safe, cheap, and has no side effects - making it the best first step for most people.
Can pregnancy cause nonallergic rhinitis?
Yes. Hormonal changes during pregnancy - especially rising estrogen - can cause nasal congestion and runny nose in 20-30% of women. This usually starts in the second trimester and resolves within two weeks after birth. It’s called pregnancy rhinitis and is a form of nonallergic rhinitis.
Should I avoid nasal decongestant sprays?
Yes - unless you’re using them for just 3-5 days. Overuse leads to rebound congestion, a condition called rhinitis medicamentosa. This can turn a mild issue into a chronic one. If you’ve been using them for weeks, stop gradually and switch to a nasal steroid under medical supervision. Recovery is possible.
What’s the most effective treatment for runny nose?
Ipratropium bromide nasal spray (Atrovent) is the most effective for runny nose alone. It reduces nasal discharge by 70-80% within 48 hours. It doesn’t help with congestion, but if dripping is your main problem, it’s the best option available.
Can nonallergic rhinitis be cured?
There’s no permanent cure yet. But symptoms can be controlled effectively in most people using trigger avoidance, saline rinses, and targeted nasal sprays. Emerging treatments like TRPV1 blockers may one day address the root cause, but for now, management is the goal - and it works well.

