Drug-Gene Interaction Checker
Check Your Medication Safety
Enter your genetic information and medication to see potential interactions based on pharmacogenomics.
Enter your information and click "Check Interaction" to see results.
Imagine taking a medication that doesn’t work-again. Or worse, one that makes you sick. For millions of people, this isn’t hypothetical. It’s their reality. Every year, over 100,000 people in the U.S. die from adverse drug reactions. Many of these cases aren’t due to mistakes. They’re due to genetics. That’s where pharmacogenomics testing comes in. It’s not science fiction. It’s happening now. And it’s changing how doctors choose your next pill.
What Pharmacogenomics Testing Actually Does
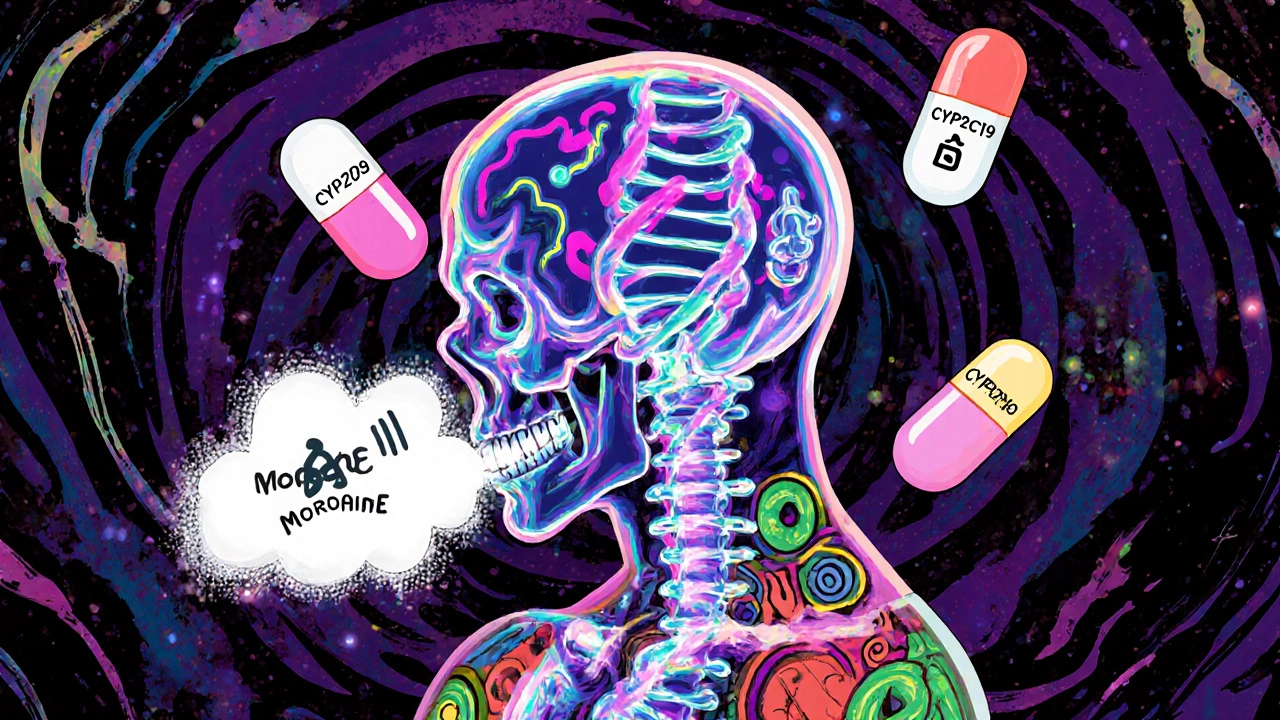
Pharmacogenomics testing looks at your DNA to predict how your body will react to certain drugs. It doesn’t tell you if you’ll get cancer. It doesn’t predict your height. It answers one simple question: Will this medication help you-or hurt you? Your genes control how fast your liver breaks down drugs. Some people process medications like a race car. Others are like a snail. That’s why two people taking the same dose of the same antidepressant can have totally different outcomes. One feels better in weeks. The other gets dizzy, nauseous, and worse. The test focuses on specific genes that affect drug metabolism. The big ones? CYP2D6, CYP2C19, and CYP2C9. These genes make enzymes that handle about 75% of all prescription drugs-from antidepressants to blood thinners to painkillers. If you’re a slow metabolizer of CYP2D6, a standard dose of codeine might not relieve your pain at all. Or worse, it could turn into toxic levels of morphine in your body. The FDA has flagged 178 drugs with genetic warnings in their labels. One of the clearest examples is abacavir, an HIV drug. If you carry the HLA-B*57:01 gene variant, you have a 50-60% chance of a life-threatening allergic reaction. Testing for this before prescribing isn’t optional anymore. It’s required.Where It’s Making the Biggest Difference
Pharmacogenomics isn’t useful for every drug. It shines where small genetic differences create huge clinical gaps. Depression treatment is one of the clearest wins. A 2022 study found that patients whose antidepressants were chosen based on their genes were 30.5% more likely to go into remission. That’s not a small improvement. That’s life-changing. One Reddit user shared how five SSRIs failed him-until his GeneSight test showed he was a CYP2D6 poor metabolizer. Switching to bupropion worked immediately. No more fatigue. No more brain fog. Just relief. Heart disease is another area. Clopidogrel (Plavix) is a common blood thinner after stents. But if you have a CYP2C19 poor metabolizer variant, your body can’t activate the drug. You’re basically taking a sugar pill. The FDA says these patients have a 50% higher risk of heart attack or stroke. Testing before prescribing can prevent that. Oncology uses it too. Tamoxifen, used for breast cancer, needs CYP2D6 to work. If you’re a poor metabolizer, the drug doesn’t convert properly. Studies show these patients have higher recurrence rates. Testing helps doctors pick alternatives like aromatase inhibitors. Even chronic pain management benefits. Opioids like oxycodone and hydrocodone are metabolized by CYP2D6. Poor metabolizers get little pain relief. Ultra-rapid metabolizers risk overdose. A single test can prevent addiction, hospitalization, or death.How the Test Works (And What It Costs)
Getting tested is simple. You spit into a tube or get a quick cheek swab. No needles. No fasting. The sample goes to a lab-usually OneOme, Invitae, or Quest Diagnostics-and results come back in 3 to 14 days. There are two main types of tests:- Targeted panels (most common): Test 5-20 key genes linked to 50-300 drugs. Cost: $250-$500.
- Whole exome or genome sequencing: Broader, but overkill for most people. Cost: $500-$2,000.
Why It’s Not Everywhere Yet
You’d think this would be standard by now. But it’s not. One reason? Doctors aren’t trained for it. A 2022 survey found only 15% of physicians feel confident interpreting pharmacogenomic reports. They don’t know how to read the results. They don’t know what to do with them. Another problem? Electronic health records (EHRs) don’t always talk to the test results. You get a report. Your doctor opens your chart. Nothing pops up. No alert. No recommendation. The data is there-but invisible. And then there’s the myth that genetics explains everything. It doesn’t. For most drugs, genes account for only 10-15% of how you respond. Age, diet, other meds, liver health, and even gut bacteria matter too. Pharmacogenomics doesn’t replace clinical judgment. It enhances it. Therapeutic drug monitoring (TDM)-measuring actual drug levels in your blood-is cheaper per test ($150-$300) and gives real-time data. But it requires repeat blood draws. Pharmacogenomics is a one-time test that tells you what to expect for life.Who Benefits Most-and Who Doesn’t
This isn’t for everyone. But it’s a game-changer for specific groups:- People who’ve tried multiple antidepressants without success
- Patients on blood thinners or heart medications after stents
- Cancer patients on tamoxifen or other metabolized drugs
- Those with chronic pain on opioids
- Anyone with unexplained side effects from medications

The Future Is Already Here
In 2023, the FDA approved OneOme’s RightMed test-the first next-generation sequencing panel for 24 genes and 350+ drugs. Epic and Cerner, the two biggest EHR systems, now automatically flag dangerous gene-drug interactions. The NIH’s All of Us program has collected genomic data from over 620,000 people-including pharmacogenomic variants-and is returning results to participants. By 2027, experts predict 30% of prescriptions will include pharmacogenomic data. Right now, it’s under 5%. That’s a six-fold increase in four years. The goal? Pre-emptive testing. Imagine getting your genes tested once-maybe as a teen or young adult-and having that data stored in your medical record. Every time a doctor prescribes a new drug, the system checks your profile and says: “This drug is risky for you. Try this instead.” The Rand Corporation estimates widespread use could save the U.S. healthcare system $137 billion a year by cutting hospitalizations and failed treatments.What You Can Do Today
If you’ve struggled with medications-especially antidepressants, painkillers, or heart drugs-ask your doctor about pharmacogenomics testing. Don’t wait for them to bring it up. Most still don’t know about it. If your doctor says no, ask for a referral to a clinical pharmacist with pharmacogenomics training. They’re more likely to understand the results and use them. If you’re paying out of pocket, choose a lab with CPIC or DPWG guidelines built into their reports. Avoid companies that sell “wellness” gene tests with no clinical validation. And remember: this isn’t about predicting your future. It’s about fixing your present. It’s about stopping the trial-and-error. It’s about getting the right drug-the first time.Is pharmacogenomics testing covered by insurance?
Medicare Part B covers testing for specific drugs like clopidogrel and abacavir. Private insurance covers about 35% of cases, mostly for psychiatric or oncology use. Most plans don’t cover general panels. Always check with your insurer before testing. Some labs offer payment plans or discounts if you pay upfront.
Can pharmacogenomics testing tell me if I’ll get addicted to opioids?
No. It can’t predict addiction. But it can tell you how your body processes opioids like oxycodone or hydrocodone. If you’re an ultra-rapid metabolizer, you may turn a normal dose into a dangerous one. If you’re a poor metabolizer, you may get no pain relief. This helps avoid ineffective or unsafe dosing-but it doesn’t predict behavior or dependence.
How long do the test results last?
Your genes don’t change. Once you’re tested, the results are valid for life. You don’t need to retake the test. Store the results in your medical record or a secure digital health app so future providers can access them.
Do I need a doctor’s order to get tested?
Yes. Most clinical tests require a provider’s order. Direct-to-consumer tests exist, but they’re often not clinically validated or covered by insurance. For reliable, actionable results, work with a doctor or pharmacist who understands pharmacogenomics.
Are there risks to getting tested?
The physical risk is zero-it’s just a saliva swab. But there are emotional and privacy risks. You might learn you’re at higher risk for side effects from a drug you’re currently taking. That can cause anxiety. Also, genetic data is sensitive. Make sure the lab follows HIPAA standards and doesn’t sell your data. Ask how they protect your information before testing.
What if my doctor ignores the results?
This happens more than you’d think. Studies show only about half of providers fully use pharmacogenomic results. If your doctor dismisses the report, ask for a referral to a clinical pharmacist specializing in pharmacogenomics. They’re trained to interpret results and can advocate for you. You can also bring a printed copy of the CPIC guidelines for your specific gene-drug pair to your appointment.

Victoria Arnett 31.10.2025
I tried pharmacogenomics after five antidepressants failed me. My CYP2D6 status came back as poor metabolizer. Switched to bupropion and suddenly I could wake up without feeling like a zombie. No more brain fog. No more crying for no reason. It’s like someone turned the lights on after years in a basement. I wish I’d done this five years ago.
HALEY BERGSTROM-BORINS 31.10.2025
Big Pharma doesn’t want this to go mainstream. Why? Because if your genes tell you which drug works, they can’t keep selling you the same ineffective pills over and over. They’re hiding this data. They’re lobbying against it. And now they’re pushing ‘wellness’ gene tests to distract you. 🤫💊👁️
Sharon M Delgado 31.10.2025
My sister, who’s a nurse in Chicago, told me about this last year-and I cried. Not because I was sad-but because I finally understood why I’d been sick for years on every painkiller they gave me. I’m a CYP2D6 ultra-rapid metabolizer. Oxycodone? Turned into morphine. I almost died. Now I take tramadol. My doctor didn’t even know about this. It’s not just science-it’s survival. Please, people-ask for this test. Please.
Dr. Marie White 31.10.2025
I’m a clinical pharmacist and I see this daily. Patients come in with stacks of failed prescriptions, and we finally run the test-and everything clicks. It’s not magic. It’s biology. But the system isn’t built to support it. EHRs don’t alert doctors. Insurance denies coverage unless you’re in oncology. And most providers still think it’s ‘experimental.’ It’s not. It’s standard in Europe. We’re behind. We need better training. And we need to stop treating genetics like a bonus feature.
Wendy Tharp 31.10.2025
So now we’re supposed to spit in a tube and let Big Pharma decide what drugs we get? Next they’ll scan our DNA and tell us who to vote for. This is just another way to control people under the guise of ‘precision medicine.’ If you’re poor metabolizer, you’re just out of luck. And guess what? You’ll still be charged $500 for the test. This isn’t science. It’s a scam dressed in lab coats.
Subham Das 31.10.2025
One must contemplate the ontological implications of pharmacogenomics within the neoliberal framework of biocapitalism. The individual, once sovereign in their corporeal autonomy, is now reduced to a genomic dataset-commodified, indexed, and monetized by corporate entities masquerading as healers. The CYP enzymes, these ancient molecular custodians of metabolic equilibrium, are now mere variables in an algorithm designed to maximize shareholder value. Is this enlightenment-or the final colonization of the human body by the logic of profit? We must awaken before our DNA becomes a subscription service.
Cori Azbill 31.10.2025
Let’s be real-this is just another way for rich white people to feel superior. You got your gene test? Cool. Now you think you’re smarter than the rest of us who just take what the doctor gives us. Meanwhile, people in India are still using turmeric for everything and living to 90. We don’t need your fancy spit tubes. We need less tech and more common sense.
Paul Orozco 31.10.2025
My cousin got this test done. The lab sent the results to his doctor. The doctor didn’t even open the PDF. Just said, ‘I’ll prescribe what I always do.’ So now he’s on a drug that made him hallucinate. And they charged him $450. This isn’t medicine. It’s a scam. They’re selling hope. And the people who need it most? Can’t afford it. And the ones who can? Don’t need it. Classic.
Ardith Franklin 31.10.2025
They say genes don’t change. But what if they do? What if stress, pollution, or that 2018 flu shot changed your methylation patterns? This test is based on static DNA-but your body isn’t static. You’re not a robot. You’re a living system. And no spit tube can capture that. This is reductionist nonsense wrapped in a white coat. Also, who authorized this? The FDA? Or the same people who approved Vioxx?
Jenny Kohinski 31.10.2025
My mom got tested after her heart stent. Turns out she’s a CYP2C19 poor metabolizer. They switched her from Plavix to ticagrelor and she’s been fine since. I’m so glad we did it. I just wish more people knew this existed. I printed the report and gave it to my own doctor. She didn’t know much either-but she looked it up after I showed her. Small wins. 😊
Aneesh M Joseph 31.10.2025
So you’re telling me I gotta pay $500 to find out if my body likes my meds? Why not just try them and see? If it makes you sick, stop. If it works, keep going. Simple. No genes needed. This is just overcomplicating stuff. I’ve been on 3 different pills and none of them killed me. So why the fuss?
Deon Mangan 31.10.2025
Ohhhhh yes. Let’s all get our DNA tested so we can avoid the *one* drug that might make us feel like a zombie. Meanwhile, 70% of Americans are on something that’s supposed to fix them but just makes them sleepy. But hey-at least now we know *why* we’re sleepy. 😌🧬
Vinicha Yustisie Rani 31.10.2025
In India, we have learned patience with healing. A medicine that does not work at first does not mean it is wrong-it means the body needs time, or another kind of care. But I respect this science. It is not magic, but it is true. I hope one day, even in small villages, people can get this test-not because it is expensive, but because it is right. The body speaks. We are learning to listen.