Medication Sweating Risk Checker
Check if your medications may be causing sweating or hot flashes. This tool identifies medications mentioned in the article and provides specific relief strategies.
More than 1 in 7 people taking certain medications experience sweating or hot flashes so bad they consider quitting their treatment. It’s not just discomfort - it’s a real reason people stop taking drugs that could save their lives. Whether it’s antidepressants, cancer meds, or painkillers, if you’re waking up soaked or suddenly feeling like you’re in a sauna, you’re not alone. And you don’t have to just live with it.
Why Your Medication Is Making You Sweat
Sweating from medication isn’t random. It’s a direct result of how the drug interacts with your body’s temperature control system. Your hypothalamus - the part of your brain that acts like a thermostat - gets thrown off by certain chemicals in pills. Some drugs overstimulate your nervous system. Others mess with hormones or trigger histamine release. The result? Your body thinks it’s overheating, even when it’s not. Antidepressants like sertraline and escitalopram are among the biggest culprits. About 1 in 5 people on these meds report excessive sweating. ADHD stimulants like Adderall and Ritalin? Up to 35% of users sweat heavily. Even common painkillers like oxycodone can trigger it through histamine release. And for women on breast cancer drugs like tamoxifen or anastrozole, hot flashes aren’t a side effect - they’re almost guaranteed. Up to 8 out of 10 patients experience them. What makes this different from regular sweating? For one, it’s usually all over your body, not just your armpits. It often happens at night, soaking your sheets. And it starts soon after you begin the drug - sometimes within days. If you’ve noticed a sudden change in sweating after starting a new prescription, that’s your clue.When Sweating Becomes a Reason to Quit
A 2021 study found that nearly 3 in 10 people stop taking their meds because of sweating. That’s not just inconvenient - it’s dangerous. Stopping antidepressants suddenly can trigger withdrawal. Skipping cancer drugs increases recurrence risk. Skipping pain meds can mean uncontrolled pain. The problem? Many doctors don’t ask about it. A 2022 study showed only 42% of primary care doctors routinely check for medication-induced sweating during follow-ups. If you’re suffering, you have to speak up. Don’t assume it’s normal. Don’t wait for your doctor to notice. Real people are dealing with this every day. One Reddit user on r/ADHD said he used to go through three undershirts a day on Adderall. Another woman on BreastCancer.org went from 20 hot flashes a day to just 3-4 after switching meds and using layered clothing. These aren’t rare cases. They’re common - and fixable.First-Line Relief: Prescription Antiperspirants
The most effective first step isn’t another pill - it’s a stronger antiperspirant. Over-the-counter brands won’t cut it. You need prescription-strength formulas with 12-20% aluminum chloride hexahydrate. Brands like Drysol or Xerac AC are the gold standard. Apply it to dry skin at bedtime, 2-3 nights a week. Don’t apply right after showering - your skin needs to be completely dry. You’ll start seeing results in about a week. Studies show it works for nearly 7 out of 10 people. It’s not glamorous, but it’s proven. A Drugs.com review of over 4,800 SSRI users found 59% got moderate to significant relief from clinical-strength antiperspirants. And unlike pills, it doesn’t affect your brain or hormones. It just blocks sweat glands where you need it.Timing Your Meds to Avoid Night Sweats
Sometimes, the fix is as simple as changing when you take your pill. If you’re on an antidepressant or stimulant that causes sweating, taking it in the morning instead of at night can cut night sweats by more than half. Why? Because the drug’s peak effect happens hours after you take it. If you take it at 8 p.m., you’re likely hitting your worst sweating phase right when you’re trying to sleep. Take it at 7 a.m., and the peak passes before bedtime. This trick works especially well for SSRIs, ADHD meds, and corticosteroids. One Cleveland Clinic study showed a 55% drop in nighttime sweating just from shifting timing. Talk to your doctor before making changes - but don’t assume you have to suffer through sleepless, soaked nights.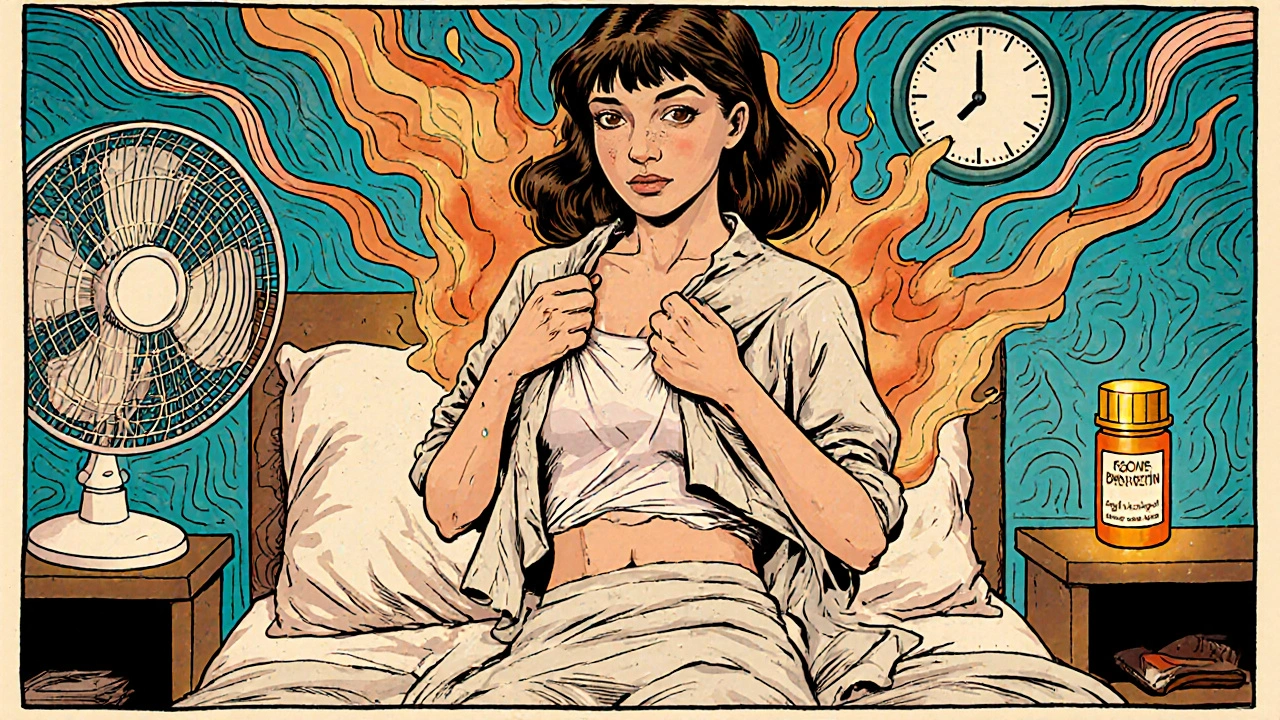
Medications to Block the Sweating
If antiperspirants and timing don’t help enough, there are oral options. Glycopyrrolate, a low-dose anticholinergic, is prescribed off-label for this exact problem. At 0.5 to 1 mg daily, it can reduce sweat episodes by over 70% in severe cases. It’s not without side effects - dry mouth, blurred vision, constipation - but for many, it’s worth it. It doesn’t interfere with your main treatment. It just turns down the sweat signal. For breast cancer patients, paroxetine (a low-dose antidepressant) is now recommended specifically to reduce hot flashes - even though it’s the same class of drug that often causes them. At 10 mg daily, it cuts hot flashes by 62%. It’s a counterintuitive fix, but it’s backed by the American Society of Clinical Oncology.Non-Drug Strategies That Actually Work
You don’t need more pills to feel better. Simple lifestyle changes can make a huge difference. Layer your clothing. Wear cotton undershirts under lightweight outer layers. That way, you can peel off a layer when you feel hot. It’s not fancy, but 92% of women in the BreastCancer.org forum say it’s their #1 tool. Keep your bedroom cool - below 65°F. Use fans. Try cooling pillows. One study found that sleeping in a cooler room reduced hot flash frequency by 84%. Cognitive behavioral therapy (CBT) designed for hot flashes isn’t just for anxiety. A 2023 Mayo Clinic trial showed that six to eight weekly sessions cut symptom severity by 50-60%. You learn to recognize triggers, reframe sensations, and breathe through flare-ups. It’s not magic - it’s training your brain to stop panicking when you feel hot. Cooling vests like the Arctic Heat model are gaining traction. Worn for two hours a day, they reduce sweat episodes by over 40%. They’re not cheap, but for people with severe symptoms, they’re life-changing.When to Ask About Switching Medications
Sometimes, the best solution is a different drug. Not all antidepressants cause sweating equally. Sertraline? High risk. Bupropion? Much lower. Not all breast cancer drugs are the same - exemestane causes fewer hot flashes than anastrozole in some women. If you’re on a medication that’s essential - like an antiretroviral, cancer drug, or blood pressure pill - don’t assume you’re stuck. Ask your doctor: “Is there an alternative with a lower risk of sweating?” A 2023 study showed that reducing the dose of problematic meds by 25% every few weeks often cuts sweating without losing effectiveness. Seven in ten patients maintained their treatment results while feeling better. Don’t let fear of change keep you suffering. Your doctor can help you weigh risks. Sometimes, switching from oxycodone to a non-opioid pain reliever reduces sweating dramatically. Sometimes, swapping an SSRI for a different class of antidepressant makes all the difference.
What’s New in 2025
The field is moving fast. In late 2023, the FDA approved Brimonidine Gel 0.33% (Mirvaso) for generalized hyperhidrosis - the first topical treatment approved specifically for full-body sweating, not just facial. Early results show a 67% reduction in sweat episodes. The NIH is also funding a $4.7 million study into genetic factors. Early data suggests some people have a gene variant (HLA-DQB1) that makes them 3.2 times more likely to sweat from meds. That could lead to personalized screening one day. Wearable tech is coming too. A device called SweatTech Smart Patch is in trials. It detects sweat before it happens and activates cooling. Think of it like a mini air conditioner on your skin. The big shift? Doctors are finally recognizing this as a real problem. The American Medical Association now recommends screening for sweating during every medication review. In oncology clinics, 82% do it. In primary care? Only 47%. That gap is closing - but you still need to speak up.What Doesn’t Work (And Why)
Avoid “natural” remedies like black cohosh or soy isoflavones for drug-induced hot flashes. Studies show they don’t work for this type - and they can interfere with cancer treatments. Avoid herbal supplements unless your doctor approves them. Don’t rely on OTC antiperspirants. They’re too weak. You need prescription strength. Don’t skip your meds just because you’re sweating. The risk of untreated depression, cancer, or pain is far greater than the discomfort of sweating. And don’t wait for your doctor to ask. If you’re sweating more than usual after starting a new drug, say something. Most doctors aren’t trained to connect the dots.What to Do Next
Start by tracking your symptoms. When do they happen? After which meds? How bad are they? Use a simple journal - even just notes on your phone. Then, talk to your prescriber. Ask these three questions:- Could this medication be causing my sweating?
- Is there a lower-risk alternative?
- Can we try a dose reduction or timing change?
- Apply prescription antiperspirant at night, 2-3 times a week.
- Take your meds in the morning if possible.
- Start wearing breathable layers and keep your bedroom cool.
Can antidepressants cause night sweats?
Yes, antidepressants - especially SSRIs like sertraline and escitalopram - cause night sweats in about 32% of users. This happens because they affect serotonin levels in the brain, which disrupts the body’s temperature control. Night sweats often improve when the medication is taken in the morning instead of at night, or when switching to a different antidepressant like bupropion.
Do all cancer drugs cause hot flashes?
No, but hormone therapies for breast cancer - like tamoxifen, anastrozole, and exemestane - cause hot flashes in up to 78% of patients. These drugs lower estrogen, which directly affects the hypothalamus. Not all cancer drugs do this - chemotherapy and immunotherapy rarely cause hot flashes unless they impact hormone levels. Switching from anastrozole to exemestane can reduce symptoms for some women.
Is sweating from medication dangerous?
The sweating itself isn’t dangerous, but the reason you’re stopping your medication because of it can be. Stopping antidepressants, cancer drugs, or heart medications abruptly can lead to serious health risks. The real danger is untreated underlying conditions. That’s why managing the sweating - not avoiding the drug - is the goal.
Can I use over-the-counter antiperspirants for medication-induced sweating?
Most over-the-counter antiperspirants won’t help enough. They typically contain only 5-10% aluminum salts. Prescription antiperspirants with 12-20% aluminum chloride hexahydrate are far more effective, cutting sweat episodes in nearly 70% of users. If OTC products aren’t working, ask your doctor for a prescription.
Will I have to take medication for sweating forever?
Not necessarily. If you can switch to a different medication that doesn’t cause sweating, the problem may disappear entirely. If you need to keep your current drug, you might only need short-term help - like using antiperspirant for a few months or taking glycopyrrolate temporarily. Many people find their bodies adjust over time, or symptoms lessen with lifestyle changes like cooling techniques and CBT.
What should I do if my doctor won’t take my sweating seriously?
Bring data. Print out the 2023 meta-analysis from the Journal of Clinical Pharmacy and Therapeutics or the American Society of Clinical Oncology guidelines on hot flash management. Say: “I’m not asking to stop my treatment - I’m asking for help managing a known side effect.” If needed, ask for a referral to a dermatologist or a specialist in medication side effects. You have a right to be heard.


Karandeep Singh 30.11.2025
Ugh why do ppl always assume meds are the issue? Could just be your diet or you’re dehydrated. Also why are we blaming pharma when it’s probably your sleep hygiene?
Suzanne Mollaneda Padin 30.11.2025
For anyone dealing with SSRI-induced hyperhidrosis: DrySol applied to armpits, chest, and back at night works better than anything else. I was soaked every night on sertraline. After 3 weeks of consistent use? Barely damp. No dry mouth, no brain fog. Just less wet sheets. Worth the prescription hassle.
Kelly Essenpreis 30.11.2025
So you’re telling me the solution is more chemicals? Antiperspirants then glycopyrrolate then paroxetine? Sounds like the pharmaceutical industrial complex just designed a new revenue stream. Wake up people
Kenny Leow 30.11.2025
Layering clothes is the real MVP. Cotton undershirt + linen shirt + light cardigan = instant temp control. I use this with Adderall and it’s life-changing. Also keep a fan on your nightstand. Simple. Cheap. No scripts needed. 🌬️
Bonnie Youn 30.11.2025
YOU ARE NOT ALONE. I was on tamoxifen and had 25 hot flashes a day. I tried everything. Then I started using a cooling pillow and took my meds at 7am. Now I’m down to 2-3. It’s not magic. It’s science. And you deserve to feel better. Don’t give up. 💪
Alexander Williams 30.11.2025
The notion that aluminum chloride hexahydrate is ‘gold standard’ is a gross oversimplification. The mechanism of action is not fully understood, and the efficacy data is largely drawn from small, non-blinded cohorts with high attrition. Moreover, the assumption that blocking eccrine glands is a therapeutic endpoint rather than a symptomatic palliation reflects a fundamental misalignment with autonomic physiology. You’re treating the biomarker, not the pathophysiology.
elizabeth muzichuk 30.11.2025
They don’t want you to know this but the FDA approved Mirvaso because Big Pharma knew people would pay $300 for a gel that ‘works’ - while the real solution - stopping the drug - is never discussed. They profit from your suffering. This isn’t medicine. It’s a business model.
Debbie Naquin 30.11.2025
What’s interesting is the neuroendocrine feedback loop here - serotonin modulation alters hypothalamic set points, but the body’s thermoregulatory plasticity can adapt over time. That’s why some users report diminished symptoms after 3–6 months. The real variable isn’t the drug - it’s individual neurophenotypic variance. We need longitudinal biomarker tracking, not just anecdotal relief metrics.
Rachel Stanton 30.11.2025
For those scared to talk to their doctor: bring this post. Print the stats. Say ‘I’m not asking to stop my treatment - I’m asking for help managing a known side effect.’ You’d be shocked how many providers just didn’t know this was common. You’re not being difficult. You’re being smart.
Mary Ngo 30.11.2025
Have you considered that the real issue isn’t the sweating - it’s the societal taboo around bodily functions? We’re taught to hide sweat, to be ‘polite’ in our discomfort. But the body is not a machine to be silenced. What if we stopped trying to suppress the symptom and started listening to what it’s telling us about our internal state? This isn’t a pharmacological problem - it’s a spiritual one.
Amber-Lynn Quinata 30.11.2025
Just tried the cooling vest. It’s expensive but worth it. I wore it for 2 hours during the day and my night sweats dropped by half. Also, I started journaling when they happen - turns out stress spikes make them worse. I didn’t realize how connected my anxiety was to this. 🤯
Lauryn Smith 30.11.2025
My mom had hot flashes from tamoxifen and she just started sleeping with a damp washcloth on her neck. Sounds silly but it worked. Also, no caffeine after noon. And she switched to bupropion. No more soaking through pajamas. You can do this.
Scotia Corley 30.11.2025
The suggestion to use glycopyrrolate is clinically irresponsible. Anticholinergics carry significant cognitive risks in patients over 50, especially with long-term use. This recommendation lacks risk-benefit analysis and ignores the Beers Criteria. Prescribing this for a non-life-threatening side effect is a failure of medical ethics.
ariel nicholas 30.11.2025
And yet… nobody mentions that the ‘FDA-approved’ Mirvaso was tested on a cohort of 112 people… and 37% reported rebound flushing… and the study was funded by Galderma… and the ‘67% reduction’ was measured via patient self-report… and the control group was given placebo cream that contained fragrance… and the primary endpoint was changed mid-trial… and…
James Allen 30.11.2025
Look, I get it - you want to feel better. But let’s be real: if you’re taking cancer meds and sweating is your biggest problem? You’re winning. I’ve seen people lose limbs from chemo. Your sheets are wet. You’re alive. Maybe stop complaining and be grateful.