Anemia and Kidney Disease: What You Need to Know About the Connection
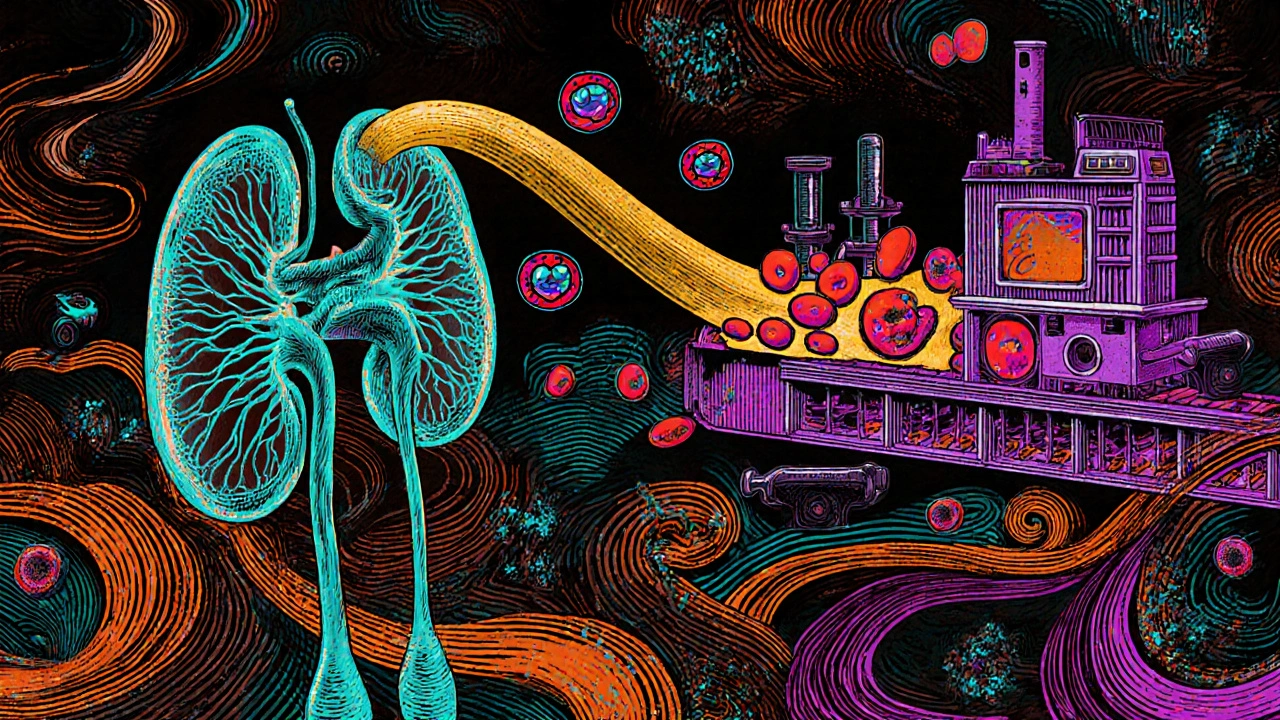
When your kidneys, organs that filter waste and help make red blood cells. Also known as renal system, they do more than just clean your blood—they signal your bone marrow to produce red blood cells. If your kidneys are damaged, that signal gets weak or stops. That’s when anemia, a condition where your body doesn’t have enough healthy red blood cells to carry oxygen. Also known as low hemoglobin, it becomes a serious side effect of chronic kidney disease, long-term damage that reduces kidney function over time. It’s not just fatigue you feel—it’s your whole body struggling to keep up.
Most people think anemia means you’re just low on iron, but with kidney disease, it’s often about erythropoietin, a hormone made by healthy kidneys that tells your body to make red blood cells. When kidneys fail, they make less of it. Even if you eat iron-rich foods or take supplements, your body still won’t produce enough red blood cells without that hormone signal. That’s why iron pills alone won’t fix it. Many people with kidney disease need injections of synthetic erythropoietin—or drugs that work like it—to get their levels back up. And even then, it’s not always simple. Inflammation from kidney disease can block iron from being used properly, making treatment trickier than it looks.
What you’ll find in the posts below isn’t just a list of treatments. It’s a real look at how kidney disease affects your body beyond the obvious—how it connects to fatigue, how medications interact with your blood cells, and why some people respond to therapy while others don’t. You’ll see how anemia isn’t just a lab number—it’s something that changes your days, your energy, and your ability to keep up with life. These articles don’t repeat the same advice. They show what actually works, what doesn’t, and what doctors often miss when they only focus on hemoglobin levels.