Anticoagulants Explained – Simple Guide
If your doctor mentioned a blood thinner, you’re probably wondering what it actually does. In plain terms, anticoagulants keep your blood from forming clots that can block veins or arteries. They don’t dissolve existing clots; they just stop new ones from popping up.
Common Types and How They Differ
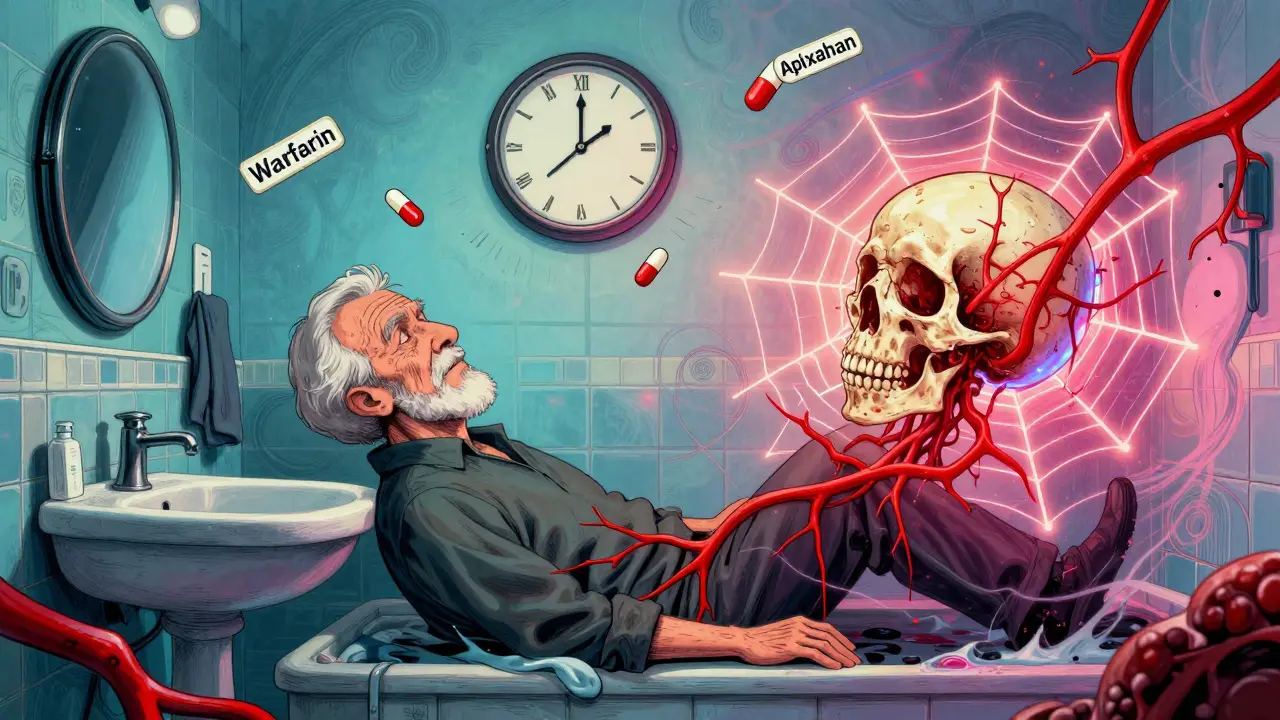
The most familiar anticoagulant is warfarin, a pill you’ve likely heard of for decades. It works by lowering vitamin K levels, which are needed for clotting. Newer options include direct oral anticoagulants (DOACs) like apixaban, rivaroxaban and dabigatran. DOACs don’t need regular blood tests, but they’re pricier and have specific kidney‑function rules.
Safe Use Tips You Should Follow
First, always take the medication exactly as prescribed – no extra doses to “stay safe.” Keep a consistent schedule; missing a dose can raise clot risk. If you’re on warfarin, your doctor will ask for INR blood tests every few weeks to make sure the level stays in range.
Second, watch out for food and drug interactions. Vitamin K‑rich foods (leafy greens, broccoli) can lower warfarin’s effect, while some antibiotics or anti‑inflammatories boost it. Over‑the‑counter pain relievers like ibuprofen also increase bleeding risk, so stick to acetaminophen unless your doctor says otherwise.
Third, carry a small card that lists all your anticoagulants and doses. If you ever need emergency care, this helps doctors avoid giving you extra blood thinners or certain surgeries without precaution.
Finally, know the signs of trouble: unusual bruising, nosebleeds that won’t stop, dark stools, or sudden severe headaches. If any of these happen, call your doctor right away – they may need to adjust your dose.
Anticoagulants are powerful tools for preventing strokes, heart attacks and deep‑vein thrombosis, but they require respect. By staying on schedule, monitoring food and drug combos, and watching for warning signs, you can reap the benefits while keeping risks low.