Iron Therapy for CKD: What Works, What Doesn’t, and Why It Matters
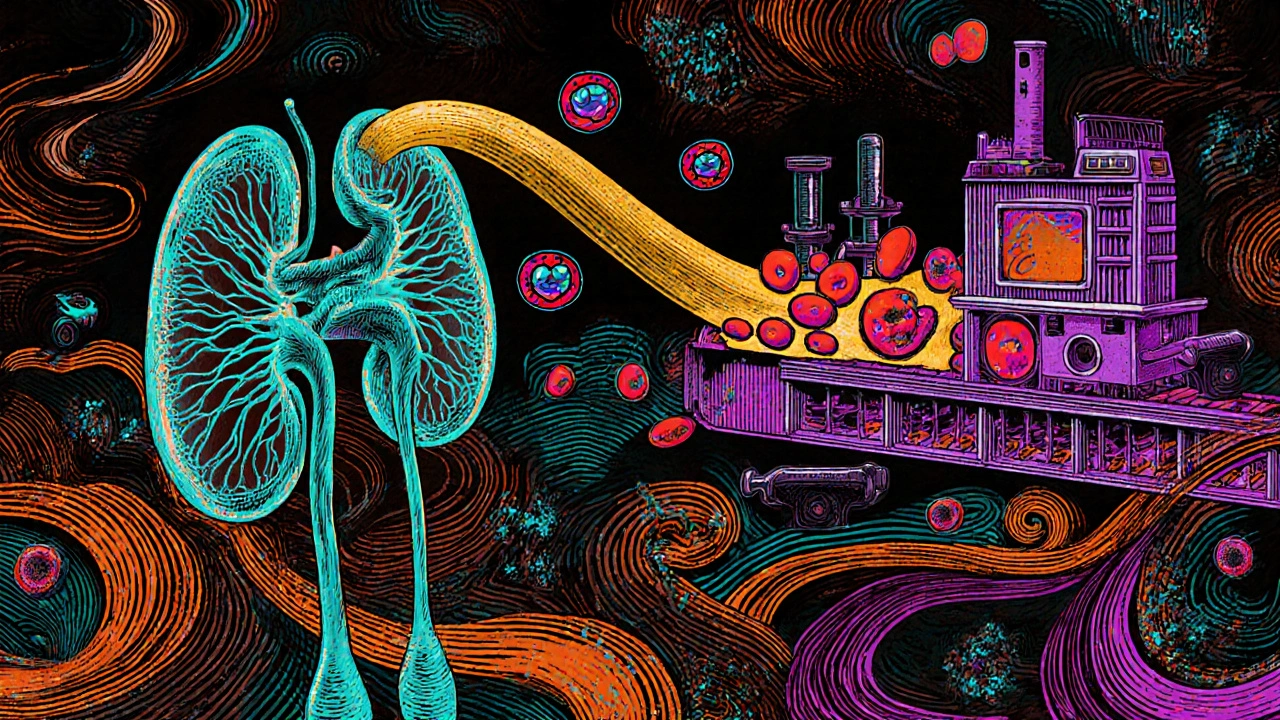
When you have chronic kidney disease, a long-term condition where the kidneys lose their ability to filter waste and regulate blood pressure. Also known as CKD, it often leads to anemia because the kidneys stop making enough erythropoietin—the hormone that tells your body to make red blood cells. This is where iron therapy, the medical use of iron supplements to restore healthy iron levels in the blood. It’s not just about eating more spinach—it’s about getting the right form, at the right time, and in the right dose.
Most people with advanced CKD, especially those on dialysis, can’t absorb oral iron well. That’s why doctors turn to intravenous iron, iron delivered directly into the bloodstream through an IV. It’s faster, more reliable, and often the only way to keep hemoglobin levels stable. But it’s not without risks—some patients get allergic reactions, low blood pressure, or even infections if the IV isn’t handled right. Oral iron, like ferrous sulfate, still has a place for early-stage CKD patients, but many give up on it because it causes stomach upset, constipation, or just doesn’t seem to work. The key isn’t just taking iron—it’s knowing iron therapy for CKD isn’t one-size-fits-all.
Iron levels don’t exist in a vacuum. They’re tied to inflammation, dialysis frequency, and whether you’re on ESA (erythropoiesis-stimulating agents) like epoetin. If your iron stores are low but your inflammation is high, giving more iron won’t help—you need to address the root cause. That’s why doctors check ferritin and transferrin saturation, not just hemoglobin. Too little iron, and you stay tired and weak. Too much, and you risk oxidative damage, heart problems, or even faster kidney decline. It’s a tightrope walk, and the goal isn’t to max out iron—it’s to find the sweet spot where your body can make red blood cells without overloading.
What you’ll find in the posts below isn’t a list of supplements or miracle cures. It’s real-world guidance from people who’ve been through this—how iron therapy affects sleep, why some patients feel worse after an IV, how diet plays a role even when you’re on dialysis, and what to ask your nephrologist before starting or stopping treatment. You’ll see how iron interacts with other meds, why timing matters with phosphate binders, and how to tell if your treatment is actually working—or just costing you money and discomfort.