Pharmaceutical Manufacturing: How Drugs Are Made and Why It Matters
When you swallow a pill, you’re trusting a complex process called pharmaceutical manufacturing, the systematic process of producing medications under strict regulatory standards to ensure safety, potency, and consistency. Also known as drug production, it’s not just mixing chemicals—it’s engineering reliability at every step, from the lab to your medicine cabinet. This process starts with active pharmaceutical ingredients, the biologically active components that make a drug work, like levothyroxine for thyroid issues or canagliflozin for diabetes. These ingredients are then combined with fillers, binders, and coatings to form tablets, capsules, or liquids. But the real challenge isn’t making the ingredient—it’s making it the same way, every single time, across millions of doses.
That’s why generic drugs, lower-cost versions of brand-name medicines that contain the same active ingredient and meet the same quality standards are so important. They’re not cheaper because they’re poorly made—they’re cheaper because they don’t carry the cost of original research. But even generics must pass the same tests for dissolution, purity, and absorption. If a generic doesn’t release its active ingredient at the same rate as the brand, it can cause real problems—like thyroid medication not working, or blood pressure drugs failing to stabilize. That’s why the FDA and other global regulators inspect manufacturing sites, review batch records, and test samples before drugs ever reach patients.
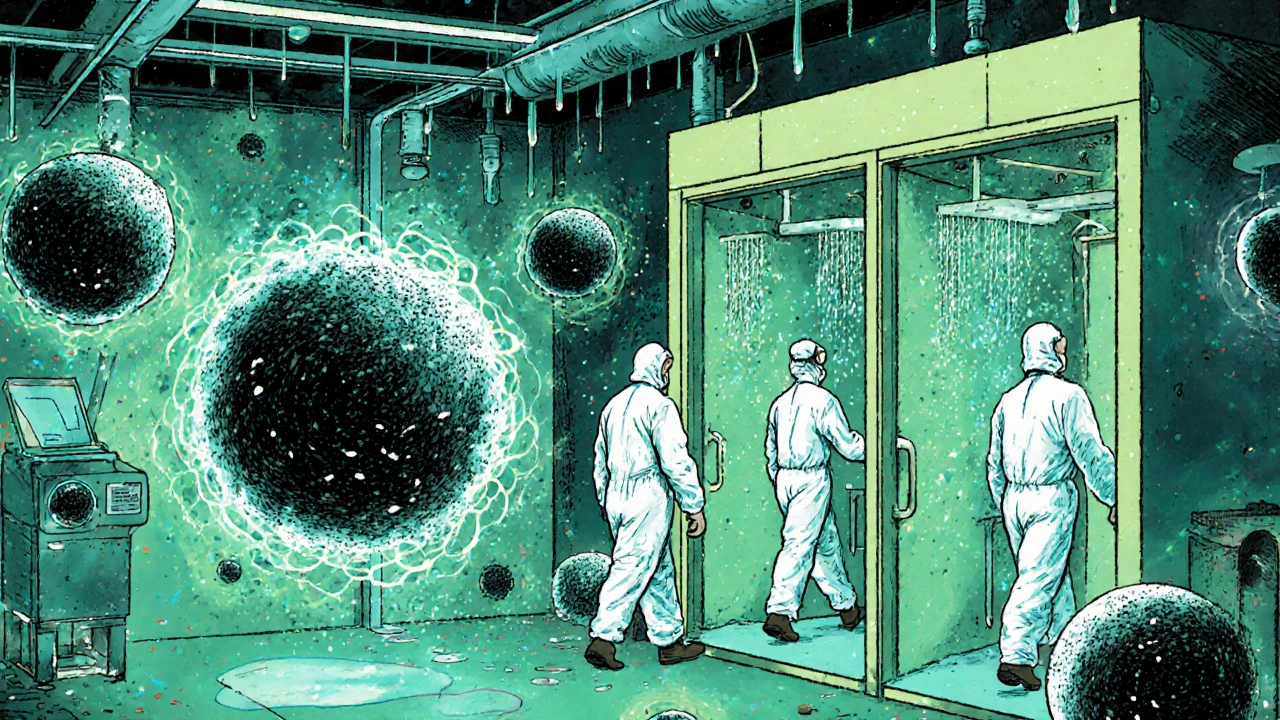
Not all manufacturing is equal. Some facilities are state-of-the-art, with robotic systems and real-time quality monitoring. Others, especially overseas, may cut corners. That’s why the source of your medication matters—not because generics are bad, but because oversight varies. The same active ingredient made in a certified U.S. plant versus an unregulated facility can have different impurities, fillers, or stability profiles. This is why you might notice differences in how a generic works for you compared to another brand, even if the label says the same thing.
Pharmaceutical manufacturing also determines how quickly new drugs reach you. Breakthrough treatments like new antidepressants or SGLT2 inhibitors don’t just appear overnight—they go through years of scale-up, where tiny lab batches are transformed into thousands of pills per hour. This is where fixed-dose combinations come in—like combining two blood pressure drugs into one pill to improve adherence. It sounds simple, but getting the right balance of ingredients, release rates, and stability is incredibly complex.
Behind every medication you take, there’s a story of chemistry, engineering, and regulation. Whether it’s the iron therapy used for kidney disease, the mesalamine for Crohn’s, or the naloxone used in overdose emergencies, each one had to be manufactured under conditions that protect your health. And when that system fails—whether through contamination, mislabeling, or poor quality control—the consequences aren’t theoretical. They’re real people with bad reactions, failed treatments, or worse.
Below, you’ll find real-world guides that connect directly to how drugs are made, tested, and delivered. From how to read medication labels for kids to why switching psychiatric drugs can trigger side effects, these posts show you how manufacturing quality touches every part of your treatment. You’ll learn what to ask, what to watch for, and how to spot when something doesn’t add up—not because you’re suspicious, but because you’re informed.