Compare Xenical (Orlistat) with Other Weight-Loss Medications
Compare Xenical (Orlistat) with other weight-loss medications like Saxenda, Wegovy, Contrave, and Alli. Learn how each works, their side effects, costs, and which is best for your goals.
When it comes to weight loss medications, prescription drugs designed to help people lose excess body fat by affecting appetite, metabolism, or fat absorption. Also known as anti-obesity medications, these aren’t magic pills—they’re tools meant for people who’ve tried diet and exercise but still struggle with stubborn weight, often due to medical reasons like hormonal imbalances or insulin resistance. Many people assume these drugs are just stronger versions of over-the-counter supplements, but that’s not true. Real weight loss medications are regulated, clinically tested, and prescribed by doctors after evaluating your health history.
Some of the most common ones include phentermine, a stimulant that reduces hunger by affecting brain chemicals like norepinephrine, and semaglutide, a GLP-1 receptor agonist originally developed for type 2 diabetes that also slows digestion and signals fullness to the brain. These aren’t interchangeable. Phentermine works fast but has a short-term use limit due to tolerance and side effects like jitteriness or high blood pressure. Semaglutide takes weeks to show results but can lead to major, sustained weight loss—up to 15% or more in some cases—when paired with lifestyle changes.
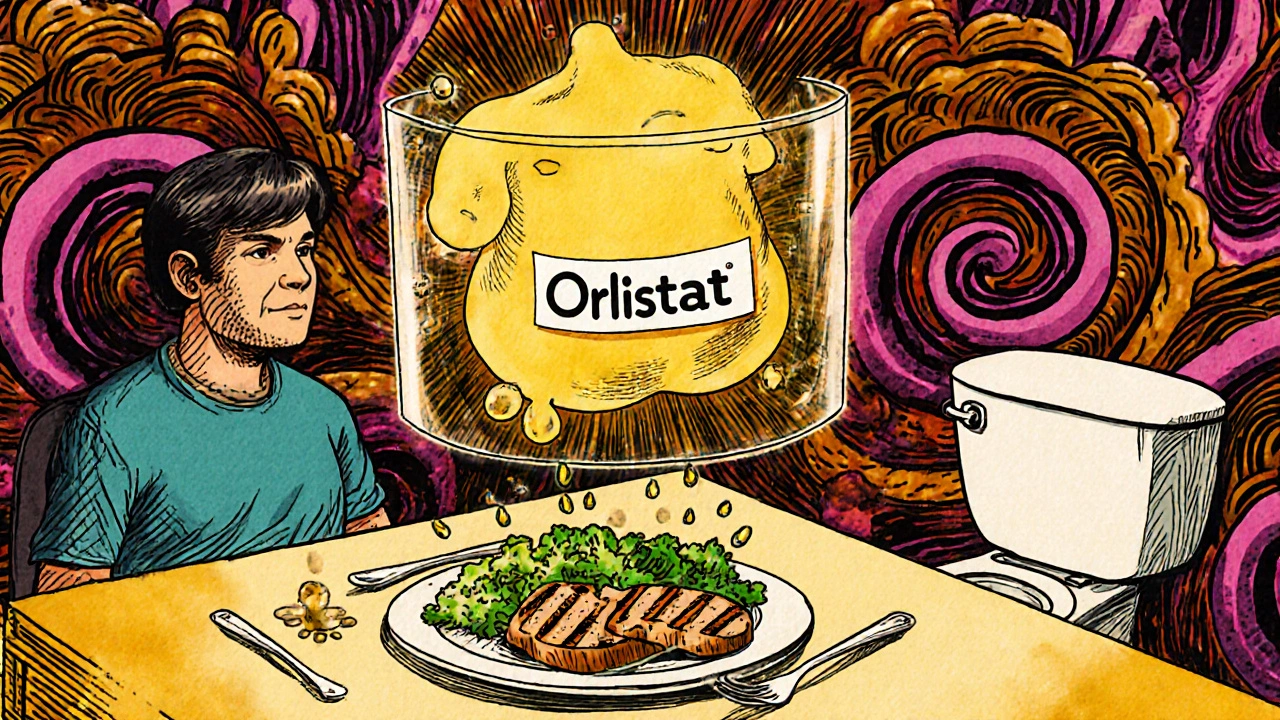
Other options like orlistat, a fat blocker that prevents your body from absorbing about 30% of dietary fat, work differently still. It doesn’t touch your appetite—it just lets unabsorbed fat pass through your system. That means greasy stools and bathroom urgency are common, which is why many people quit using it. Then there’s liraglutide, another GLP-1 drug similar to semaglutide but with a higher daily injection frequency, and newer ones like tirzepatide, a dual GIP/GLP-1 agonist showing even stronger results in trials. Each has its own profile: cost, dosing, side effects, and how well it fits your body’s biology.
What these drugs don’t do is replace healthy habits. You can’t eat junk food and expect a pill to fix it. They’re meant to help you stick to a plan—not create one. People who combine these medications with regular movement, protein-rich meals, and sleep hygiene tend to keep the weight off longer. Those who stop the drug without changing their lifestyle often regain everything, sometimes even more.
Side effects vary. Nausea is common with GLP-1 drugs, especially at first. Some report headaches, dizziness, or dry mouth. Rare but serious risks include pancreatitis, gallbladder disease, or thyroid tumors in animal studies (no proven link in humans yet). That’s why you need a doctor’s oversight—not a random online pharmacy. These aren’t supplements you order with free shipping.
What you’ll find in the posts below is a collection of real comparisons, side-by-side breakdowns, and honest takes on how these drugs stack up against each other—and against lifestyle changes. No fluff. No marketing spin. Just clear facts on what’s actually been studied, who it helps most, and what to watch out for. Whether you’re considering a prescription, wondering why your friend lost weight on semaglutide, or just trying to understand the hype, this guide cuts through the noise.
Compare Xenical (Orlistat) with other weight-loss medications like Saxenda, Wegovy, Contrave, and Alli. Learn how each works, their side effects, costs, and which is best for your goals.