IC Symptom Assessment Tool
This tool estimates your likelihood of interstitial cystitis (IC) based on symptoms described in the article. The O'Leary-Sant Symptom Index scores your urinary and pelvic symptoms on a scale of 0-24, with 8+ indicating possible IC.
Your score will appear here after calculation.
When women experience vaginal burning is a sharp, irritating sensation in the vaginal area that can flare up during urination, intercourse, or even at rest, they often wonder why it happens and whether it’s something serious. One condition that frequently shows up in the background is interstitial cystitis is a chronic bladder disorder marked by pelvic pain, urgency, and frequency without a bacterial infection. Understanding how these two issues intersect can save you from months of confusion and help you get the right care faster.
Key Takeaways
- Vaginal burning can be a symptom of many conditions, but when it co‑exists with bladder‑related pain, interstitial cystitis (IC) should be considered.
- Both IC and common vaginal infections share triggers like acidity, stress, and pelvic floor tension.
- Accurate diagnosis often requires a combination of symptom review, urine tests, and sometimes a cystoscopy.
- Treatment may involve diet changes, bladder‑training exercises, and targeted medications that address both urinary and vaginal discomfort.
- Seeing a uro‑gynecologist early can prevent chronic pain and improve quality of life.
What Is Vaginal Burning?
Vaginal burning is a localized feeling of heat, sting, or soreness inside the vaginal canal. It can arise from:
- Infections such as yeast infection is a Candida overgrowth that creates itching, redness, and a burning sensation or bacterial vaginosis is a shift in vaginal flora that leads to discharge and irritation.
- Dryness caused by hormonal changes, especially during menopause or after childbirth.
- Allergic reactions to soaps, condoms, or feminine hygiene products.
- Mechanical irritation from tight clothing, sexual activity, or prolonged sitting.
Usually, the burning is limited to the vaginal walls and eases once the underlying cause is treated.
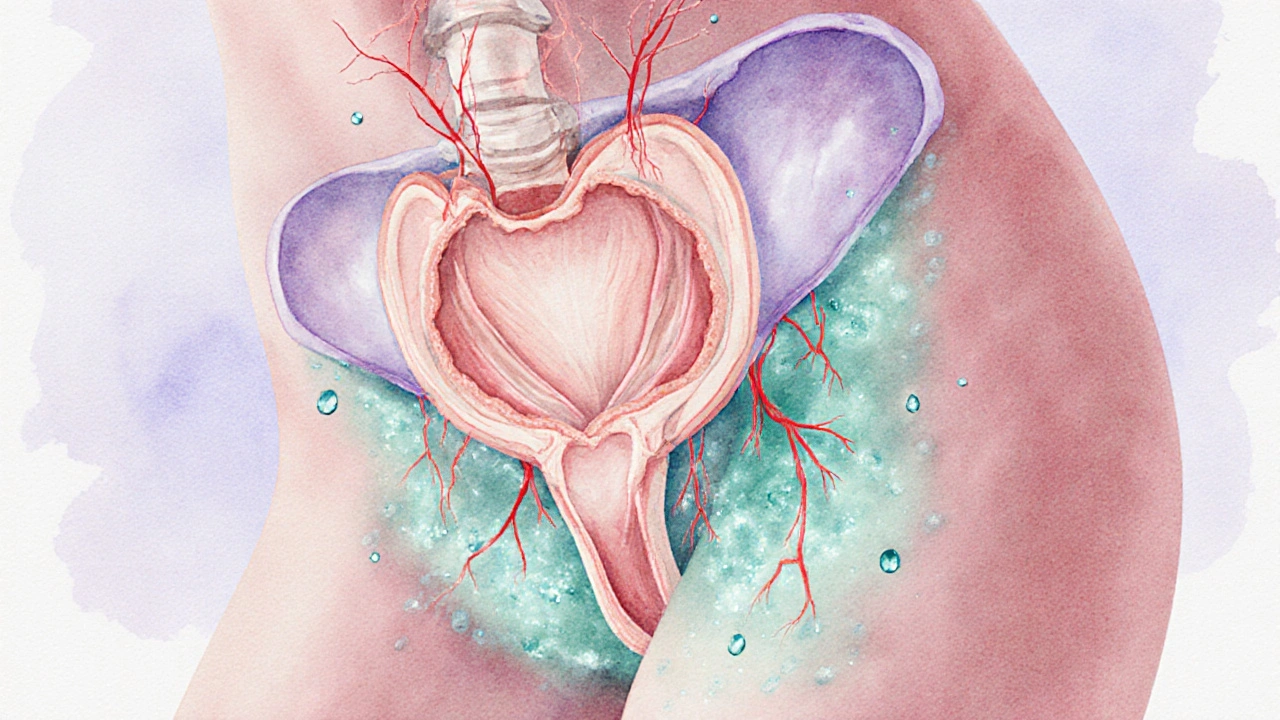
Understanding Interstitial Cystitis
Bladder pain syndrome is a broader term that includes interstitial cystitis and describes chronic pelvic discomfort linked to the bladder. IC is characterized by:
- Persistent pressure or pain in the pelvic region, often described as a dull ache or stabbing pain.
- Urinary urgency and frequency, sometimes up to 20 times a day, without signs of infection.
- Pain that worsens as the bladder fills and eases after emptying.
The exact cause remains unclear, but research points to a compromised bladder lining, abnormal nerve signaling, and possible autoimmune components.
How The Two Conditions Overlap
At first glance, vaginal burning and interstitial cystitis seem unrelated-one feels external, the other internal. Yet they share several pathways:
- Acidic environment: Both the vagina and bladder thrive at a slightly acidic pH. When the balance shifts-due to diet, infection, or inflammation-the lining becomes more sensitive.
- Pelvic floor dysfunction: A tight or spastic pelvic floor can squeeze both the urethra and vaginal walls, amplifying pain signals. This dysfunction often co‑exists with IC.
- Neuropathic sensitization: Chronic irritation can cause the nerves in the pelvis to become hyper‑responsive, meaning a mild stimulus triggers burning in both areas.
- Stress and hormonal fluctuations: Stress hormones like cortisol can lower the bladder’s protective mucus and thin vaginal epithelium, making both sites vulnerable.
Because of these shared mechanisms, many patients report that treating one side of the equation-say, improving bladder health-also eases vaginal burning.
Spotting the Signs That Link Them
When you notice a combination of the following, IC might be the hidden factor behind your vaginal burning:
- Burning that intensifies during or after urination.
- Frequent nighttime trips to the bathroom (nocturia) paired with vaginal irritation.
- Pelvic pressure that doesn’t fully disappear after emptying the bladder.
- Negative urine cultures-meaning no standard infection is found despite symptoms.
Doctors often use a symptom scoring system called the O'Leary‑Sant Interstitial Cystitis Symptom Index to quantify the overlap.
When to See a Healthcare Provider
If any of the following apply, schedule an appointment with a uro‑gynecologist or a specialist in pelvic pain:
- Burning persists for more than two weeks despite over‑the‑counter treatments.
- You experience urgency, frequency, or pain that disrupts daily activities.
- Home urine tests repeatedly come back negative, yet symptoms continue.
- You have a history of recurrent urinary tract infections (UTIs) that never fully clear.
The clinician may order:
- A potassium sensitivity test is a procedure where a dilute potassium solution is instilled into the bladder to gauge nerve sensitivity; a painful reaction suggests IC.
- A cystoscopy is a visual exam of the bladder interior using a tiny camera, often revealing characteristic glomerulations in IC patients.
- Urine culture and cytology to rule out infection or cancer.
Treatment Options That Address Both
Managing the overlap focuses on calming the nerves, restoring protective layers, and easing muscle tension.
- Pain‑relief meds: Oral pentosan polysulfate sodium (PPS) helps rebuild the bladder’s GAG layer; some patients also benefit from low‑dose tricyclic antidepressants that modulate pain signals.
- Topical therapies: A vaginal estrogen cream can improve mucosal health, reducing burning while also supporting the urethral lining.
- Dietary tweaks: Cutting out acidic foods (citrus, tomatoes, coffee) and artificial sweeteners often lessens both bladder and vaginal irritation.
- Pelvic floor physical therapy: Skilled therapists teach relaxation techniques, biofeedback, and gentle stretching that relieve tension affecting both sites.
- Bladder training: Timed voiding and gradual extension of intervals can retrain bladder capacity, lowering urgency and freeing the pelvic floor.
In refractory cases, doctors may explore Botox injections into the bladder wall or neuromodulation devices that interrupt pain pathways.
Quick Comparison: Vaginal Burning Causes vs. Interstitial Cystitis
| Feature | Typical Vaginal Burning | Interstitial Cystitis |
|---|---|---|
| Pain location | Inside vaginal canal, often localized | Pelvic floor, bladder base, may radiate to vagina |
| Trigger by urination | Occasional stinging after voiding | Burning intensifies during bladder filling and emptying |
| Frequency of urination | Usually normal | Increased (day/night), urgency |
| Response to antibiotics | Often improves if infection present | No benefit-antibiotics ineffective |
| Pelvic floor tension | May be present but not primary driver | Common contributing factor |
| Diagnostic tests | Wet prep, culture, pH test | Potassium sensitivity, cystoscopy, symptom index |
Lifestyle Tips to Reduce Discomfort
- Stay well‑hydrated but avoid bladder irritants like caffeine and artificial sweeteners.
- Wear breathable cotton underwear and avoid tight leggings that trap moisture.
- Practice gentle pelvic floor stretches-child’s pose, happy baby, and diaphragmatic breathing.
- Keep a symptom diary noting food, stress levels, and bathroom patterns; patterns often emerge.
- Consider probiotic supplements that contain Lactobacillus strains to balance vaginal flora.
Frequently Asked Questions
Can a yeast infection cause vaginal burning that feels like interstitial cystitis?
Yeast infections produce intense itching and a burning sensation, but they usually don’t cause urinary urgency or frequent nighttime trips. If you notice bladder‑related symptoms alongside the burn, it’s worth investigating IC as a co‑existing issue.
Is interstitial cystitis treatable, or is it a lifelong condition?
IC is chronic, meaning it can flare up over many years, but most patients achieve significant relief with a combination of diet changes, pelvic floor therapy, and medication. The goal is symptom control rather than a cure.
Do over‑the‑counter pain relievers help with both conditions?
NSAIDs can dull pelvic pain temporarily, but they don’t address the underlying bladder lining issue or vaginal flora imbalance. For lasting relief, targeted therapies are needed.
What role does stress play in worsening vaginal burning and IC?
Stress releases cortisol, which can thin the protective mucus in both the bladder and vagina, making nerves more exposed. Managing stress through mindfulness, yoga, or counseling often reduces symptom severity.
Should I avoid all acidic foods if I have both conditions?
Complete avoidance isn’t necessary for everyone, but reducing high‑acid items (citrus, tomatoes, carbonated drinks) can lessen irritation. Try an elimination diet for two weeks and re‑introduce foods gradually to see what triggers you.


Ryan Pitt 13.10.2025
Hang in there, managing diet and stress can really calm both the bladder and vaginal irritation.
Brian Rice 13.10.2025
It is intellectually dishonest to conflate occasional dysuria with a chronic interstitial cystitis diagnosis without rigorous cystoscopic evidence, and the article insufficiently emphasizes the necessity of differential diagnosis.
Stan Oud 13.10.2025
Many patients experience overlapping symptoms and the key is to systematically rule out infection before labeling it as IC.
Ryan Moodley 13.10.2025
While the author paints a tidy correlation, the reality is that pelvic pain is a labyrinthine construct, and attributing vaginal burning to bladder pathology oversimplifies the neuro‑vascular symphony at play.
Pradeep kumar 13.10.2025
From a pathophysiological standpoint, the acid‑base equilibrium disruption in the uro‑vaginal microenvironment can precipitate mucosal hypersensitivity, thereby synergizing IC and vulvar dysesthesia.
James Waltrip 13.10.2025
One must suspect that the pharmaceutical lobby suppresses the true prevalence of bladder–vaginal cross‑sensitization, preferring to market isolated treatments rather than embracing holistic protocols.
Kevin Napier 13.10.2025
Try keeping a symptom diary that logs foods, stress levels, and bathroom trips; patterns often surface that guide both dietary tweaks and pelvic floor therapy.
Sherine Mary 13.10.2025
Clinically, a negative urine culture coupled with nocturia and pelvic pressure is a classic red flag for interstitial cystitis, not merely a coincidental finding.
AARON KEYS 13.10.2025
Accurate diagnosis typically involves a combination of symptom indices, potassium chloride testing, and sometimes cystoscopy to visualize glomerulations.
Summer Medina 13.10.2025
Most people think that a simple diet change will fix everything but the reality is far more complex. The bladder lining is a delicate barrier that can be compromised by acids and stress. When that barrier is weakened the nerves become hyperactive and you feel burning in the vagina. This is not a myth it is documented in several urology studies. You also have to consider pelvic floor tightness that can trap pressure and worsen symptoms. Stress hormones like cortisol thin the mucus layers in both the bladder and the vagina. A healthy lifestyle can mitigate some of these factors but it is not a cure. Hydration is important yet you must avoid caffeine and artificial sweeteners that irritate the bladder. Probiotic supplements can help balance the vaginal flora and reduce inflammation. Physical therapy that targets the pelvic floor can relax the muscles and reduce nerve firing. Some patients find relief with bladder instillations of alkalinizing solutions. Others benefit from low dose tricyclic antidepressants that modulate pain pathways. The key is to adopt a multimodal approach rather than rely on a single remedy. Keep a detailed symptom journal to track triggers and progress. Consult a uro‑gynecologist who can guide you through appropriate testing. Remember that patience and consistency are essential for long‑term improvement.
Melissa Shore 13.10.2025
While the interplay between urothelial inflammation and vaginal mucosal sensitivity is complex many clinicians still rely on empirical treatment pathways. Patients often report temporary relief after dietary modifications and pelvic floor relaxation but relapse is common without ongoing maintenance. The literature suggests that combination therapy, including topical estrogen and bladder instillations, yields better outcomes than monotherapy. Moreover, regular follow‑up with a uro‑gynecologist can identify subtle changes early and prevent chronic progression.
Pradeep kumar 13.10.2025
In addition to the diary, integrating biofeedback can objectively quantify pelvic floor tension and enhance therapeutic outcomes.
Sherine Mary 13.10.2025
Moreover, the alleged suppression narrative overlooks the rigorous peer‑review process that validates interstitial cystitis protocols.
Michelle Pellin 13.10.2025
Nevertheless, the clinical community continuously refines diagnostic criteria, ensuring patients are not left in diagnostic limbo.
April Conley 13.10.2025
Bottom line, prioritize evidence‑based interventions over anecdotal myths.