Every year, tens of thousands of children under five end up in the emergency room because they accidentally swallowed medicine meant for adults. It’s not because parents are careless-it’s because the risks are hidden in plain sight. A bottle left on the nightstand. A teaspoon used instead of the dosing cup. A child-resistant cap that wasn’t fully twisted shut. These aren’t rare mistakes. They’re common, preventable, and often deadly.
Why Young Kids Are at Highest Risk
Children under five are naturally curious. They explore the world by touching, tasting, and grabbing everything within reach. Medications, especially colorful liquids, can look like candy. A bottle of children’s acetaminophen with a sweet flavor? To a toddler, it’s not medicine-it’s a treat. According to CDC data, liquid acetaminophen and diphenhydramine (an antihistamine) caused more than 40% of all pediatric medication overdoses in 2022. These aren’t rare drugs-they’re in nearly every home.The problem isn’t just access. It’s confusion. Many parents don’t realize there are different concentrations of the same medication. Infant drops are six times stronger than children’s liquid. Using the wrong one can mean giving a child five times the right dose. A 2023 study in US Pharmacist found that 42.6% of dosing errors happened because caregivers mixed up these formulations.
The PROTECT Initiative: A National Strategy That Works
In 2008, the CDC launched the PROTECT Initiative-a coordinated effort to cut pediatric medication overdoses. It’s not just a slogan. It’s a set of proven, science-backed actions that have already reduced emergency visits by 25% between 2010 and 2020.PROTECT works in three ways:
- Packaging that actually works: Child-resistant caps must be twisted until they click. But not all caps are equal. Some are easy for kids to open by age 3.5 years. The initiative pushed manufacturers to add flow restrictors-small plastic inserts that limit how much liquid can pour out. As of 2023, 95% of liquid medications now use mL-only labeling, cutting confusion from teaspoons to milliliters.
- Standardized dosing tools: Never use a kitchen spoon. Ever. A teaspoon holds 5 mL. A tablespoon holds 15 mL. But many spoons vary wildly. The dosing cup or syringe that comes with the medicine? That’s the only tool you should use. The CDC found that 78.3% of dosing errors involved kitchen utensils.
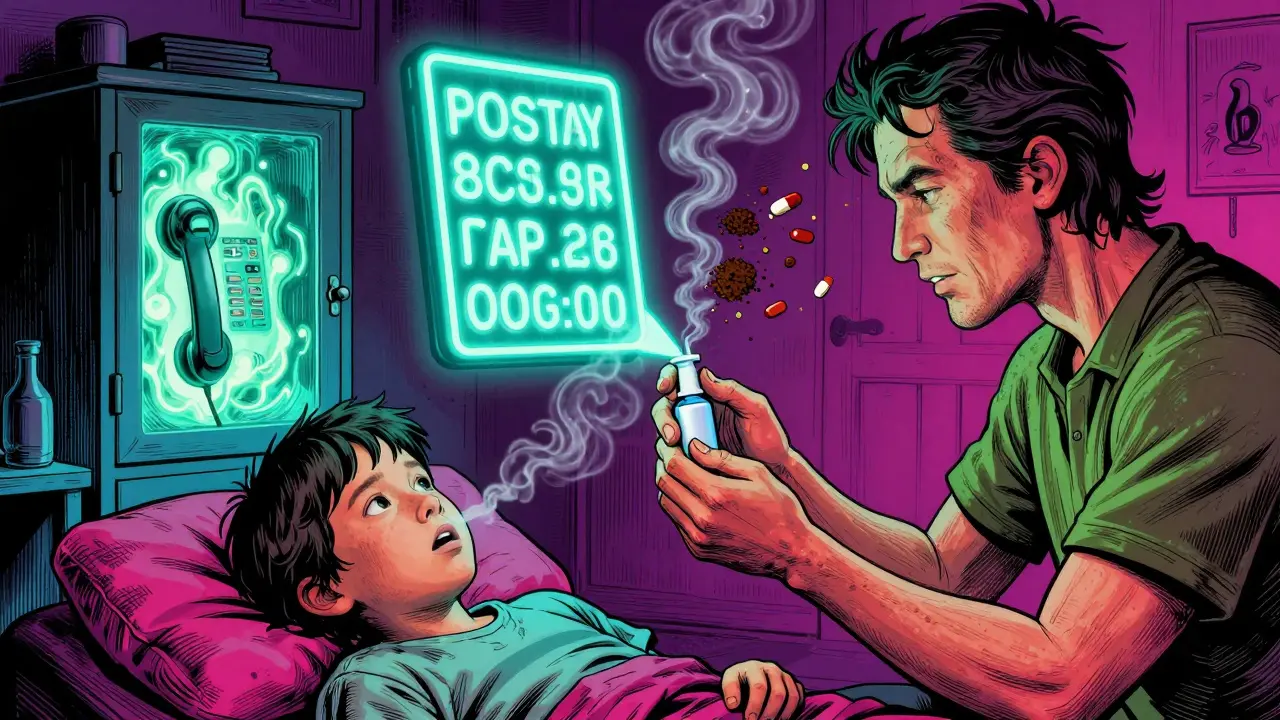
- Education that sticks: The Up and Away and Out of Sight campaign tells parents: lock it up. Keep all meds in a locked cabinet, at least 4 feet off the ground. Don’t leave pills on the nightstand after a doctor’s visit. One parent on Reddit shared how their 2-year-old got into blood pressure meds left on the dresser. They didn’t know it could be fatal. Now they lock everything.
What ‘Child-Resistant’ Really Means
Many parents think child-resistant means child-proof. It doesn’t. The Consumer Product Safety Commission tested thousands of caps and found that 10% of children can open them by age 42 months. That’s just over 3 years old. A child who can climb onto a counter or open a drawer doesn’t need to break a lock-they just need to twist.That’s why storage matters more than packaging. Even the best cap won’t help if the bottle is sitting on the bathroom counter. A 2022 survey of 5,000 U.S. households found that only 32% store medications in locked cabinets. The rest rely on high shelves or closed drawers. Those aren’t enough. Toddlers are climbers. They pull things down. They open cabinets. They find what they shouldn’t.

What to Do If Your Child Swallows Medicine
If you suspect your child took medicine they shouldn’t have, don’t wait. Don’t call your pediatrician first. Don’t Google symptoms. Call poison control immediately: 1-800-222-1222. It’s free, available 24/7, and staffed by experts who know exactly what to do.While you wait for help, do this:
- Keep the medicine bottle. The label has the active ingredients and strength-critical info for responders.
- Don’t make your child vomit. It can cause more harm.
- If it’s an opioid (like oxycodone or hydrocodone) and your child is unresponsive or not breathing, give naloxone if you have it. The SAMHSA Overdose Prevention Toolkit confirms naloxone is safe for children. It’s not just for adults.
Some families now keep naloxone at home, especially if a child is prescribed opioids after surgery. The American Academy of Pediatrics now recommends co-prescribing naloxone with any opioid for children. But only 1 in 3 pediatricians do it. That’s a gap. If your child is on opioids, ask for naloxone. Know how to use it. Practice with the trainer device.
Why Storage Isn’t Enough-Disposal Matters Too
Leftover pills are a silent threat. A 2023 study showed that 68% of unused medications stay in homes for months. Kids find them. Teens take them. Grandparents mix them up. The PROTECT Initiative pushes for safe disposal: take-back programs at pharmacies or hospitals. But only 14 states have consistent programs.If there’s no take-back option, here’s what to do:
- Remove pills from their original bottle.
- Mix them with coffee grounds, cat litter, or dirt.
- Put them in a sealed plastic bag.
- Throw them in the trash.
Never flush pills unless the label says to. Water contamination is a real issue. But mixing with unappealing substances and tossing in the trash? That’s the safest bet for most homes.
The Tools That Could Help-But Don’t Reach Everyone
Smart pill dispensers like Hero Health and AdhereIT can lock meds, send alerts, and dispense the right dose at the right time. They’re FDA-cleared. They work. But they cost $200-$500. A 2023 AAP analysis found 87% of low-income families can’t afford them. That’s not a solution-it’s a privilege.Meanwhile, basic tools are free: the dosing syringe that comes with the medicine, a locked cabinet, and poison control’s number saved in your phone. These aren’t fancy. But they save lives.
What’s Next? The Road to Zero Overdoses
The CDC’s Healthy People 2030 goal is to reduce pediatric medication overdoses by 10% from 2019 levels. By 2023, they’d already hit 6.2%. That’s progress. But it’s not enough.Upcoming changes could make a big difference:
- In 2025, the FDA will require flow restrictors on all liquid opioid medications.
- The Up and Away campaign will launch in 12 new languages by 2026.
- The American Society of Health-System Pharmacists will release its first pediatric medication safety guide in late 2024.
Each of these steps targets a real gap. But they won’t help if parents don’t know about them. That’s why education is still the most powerful tool.
Simple Rules That Save Lives
Here’s what every parent, grandparent, and caregiver should do today:- Keep all medications-prescription, OTC, vitamins-in a locked cabinet, at least 4 feet high.
- Use only the dosing tool that came with the medicine. Never a spoon.
- Read the label. Check if it’s infant or children’s formula. Never guess.
- Put medicine away immediately after use. Don’t leave it on the counter.
- Save 1-800-222-1222 in your phone. Write it on the fridge.
- If your child is prescribed opioids, ask for naloxone. Learn how to use it.
- Dispose of unused meds properly. Don’t hoard them.
These aren’t suggestions. They’re the difference between a scare and a tragedy. You don’t need a PhD to prevent this. You just need to be consistent. One locked cabinet. One dosing syringe. One saved number. That’s all it takes.
What should I do if my child swallows medicine they shouldn’t have?
Call poison control immediately at 1-800-222-1222. Do not wait for symptoms. Keep the medicine bottle handy-its label has critical info. Do not make your child vomit. If it’s an opioid and your child is unresponsive or not breathing, give naloxone if you have it. Emergency responders need to know exactly what was taken and how much.
Are child-resistant caps enough to keep kids safe?
No. Child-resistant means it’s harder to open-not impossible. Studies show 10% of children can open these caps by age 3.5. Many kids climb, open drawers, or pull down bottles from shelves. That’s why storage in a locked cabinet at least 4 feet high is essential. Packaging helps, but it’s not a substitute for safe storage.
Can I use a kitchen spoon to give liquid medicine?
Never. Kitchen spoons vary wildly in size. A teaspoon might hold 3 mL or 7 mL. The dosing syringe or cup that comes with the medicine is calibrated in milliliters (mL)-the only accurate unit. Using a spoon is the most common cause of dosing errors, accounting for nearly 80% of cases according to the National Poison Data System.
Why do some medications have different concentrations for infants and children?
Infant drops are more concentrated because babies need smaller volumes. For example, infant acetaminophen is 80 mg per 0.8 mL, while children’s liquid is 160 mg per 5 mL. If you use the infant drops with the children’s dosing cup, you could give five times the intended dose. Always check the label for concentration and use the right tool for the right formula.
Is naloxone safe for young children?
Yes. Naloxone is approved by the FDA for use in children and is included in the SAMHSA Overdose Prevention Toolkit. It reverses opioid overdoses quickly and safely. If your child is prescribed an opioid for pain, ask your doctor for naloxone. Keep it in your home. Learn how to use the nasal spray or auto-injector. It could save their life.
How do I safely dispose of unused medications?
Use a drug take-back program if one is available at your pharmacy or hospital. If not, remove pills from the bottle, mix them with coffee grounds, cat litter, or dirt, put them in a sealed plastic bag, and throw them in the trash. Never flush them unless the label says to. This prevents accidental ingestion and environmental harm.
Why do pediatricians sometimes forget to talk about safe medication storage?
A 2022 American Academy of Pediatrics survey found only 63% of pediatricians consistently discuss safe storage during well-child visits. Time, lack of training, or assumptions that parents already know can lead to gaps. Don’t wait for your doctor to bring it up. Ask: ‘How do I store my child’s medications safely?’ It’s a simple question with life-saving answers.


Milla Masliy 12.01.2026
Just read this and immediately locked up all our meds. I used to leave the Tylenol on the nightstand because ‘it’s just baby medicine’-turns out, it’s not just medicine, it’s candy to a toddler. 🥲 Thanks for the wake-up call. I’m printing out the poison control number and taping it to the fridge today.
Also, I had no idea infant drops were 6x stronger. My cousin’s kid ended up in the ER last year because of this. We all thought we were being careful. We weren’t.
Damario Brown 12.01.2026
lol so now we’re blaming parents for not being robot nannies? like wow. next you’ll say we should install biometric locks on our medicine cabinets. also why is everyone acting like 80% of dosing errors are from spoons? i used a damn measuring spoon and my kid still got into the bottle. it’s not the spoon, it’s the fact that kids are tiny little thieves with zero respect for boundaries. also why is this post 5000 words? i’m not a pharmacist.
also the word ‘PROTECT’ is in all caps like it’s a cult. 🤡
sam abas 12.01.2026
Let’s be real - the CDC’s ‘PROTECT Initiative’ is just PR fluff wrapped in jargon. You think a flow restrictor stops a 3-year-old who can climb on a chair, pull down a cabinet, and twist open a bottle with their teeth? That’s not science - that’s wishful thinking. And don’t get me started on ‘never use a kitchen spoon.’ You know what’s more accurate than a dosing syringe? A calibrated oral syringe from a pharmacy, not the cheap plastic crap that comes with the bottle. That thing leaks, bends, and gets lost in 3 days. Meanwhile, the real problem? Parents don’t read labels because they’re exhausted. You can’t fix systemic fatigue with a pamphlet.
Also, why is naloxone for kids even a thing? Opioids shouldn’t be prescribed to toddlers in the first place. Fix the root cause, not the symptom. And why are we spending millions on smart pill dispensers that cost $500? We need universal healthcare, not luxury baby tech.
Also - coffee grounds? Really? That’s your disposal method? You think that stops a determined 4-year-old? They’ll dig through trash like raccoons. This whole post is a bandaid on a gunshot wound.
Adam Vella 12.01.2026
The structural vulnerability in pediatric medication safety lies not in the pharmacokinetics of acetaminophen or the mechanical integrity of child-resistant caps, but in the epistemological dissonance between public health messaging and domestic behavioral norms. The notion that ‘locking it up’ is sufficient presumes a level of cognitive continuity and environmental control that is neither universally accessible nor consistently maintained. The socio-economic stratification of medication safety infrastructure - where smart dispensers are luxury goods and dosing syringes are disposable afterthoughts - reveals a systemic failure to equitably distribute preventative knowledge. One cannot advocate for behavioral compliance without addressing material precarity. The PROTECT Initiative, while empirically sound, remains an ideological construct divorced from the lived realities of caregivers operating under chronic stress, resource scarcity, and institutional neglect. Until policy aligns with practice - not just pamphlets - we are merely performing safety, not ensuring it.
Clay .Haeber 12.01.2026
Oh wow. So now we’re treating parents like criminals because they didn’t install a vault in their bathroom? 🙄
Let me guess - the next article will be ‘How to Prevent Your Toddler From Drinking Your Coffee’? Because apparently, we’re all just one unattended bottle away from a tragedy. Can we at least agree that if your kid is climbing on counters to get medicine, maybe you need a new parenting strategy? Or maybe - just maybe - your child is a tiny, terrifying genius who’s already outsmarted you?
Also, ‘never use a kitchen spoon’? Cool. So now I’m supposed to carry a syringe in my purse like I’m a diabetic ninja? I’m not a pharmacist. I’m a mom who just wants to give my kid Tylenol without becoming a full-time safety inspector.
And who the hell thought coffee grounds were a good disposal method? That’s just giving your trash a weird, bitter personality. Next time, just flush it. The ocean doesn’t care.
vishnu priyanka 12.01.2026
Man, this hits different. In India, we don’t even have proper labels on meds sometimes - just scribbles in Hindi or Tamil. I saw a kid swallow a whole bottle of cough syrup because the bottle looked like juice. No caps, no warnings, just a plastic bottle with a cap that popped off with one twist.
But here’s the thing - we don’t have locked cabinets either. We keep meds on shelves because we don’t have space. So yeah, this post is right - but it’s also kinda… American? We need solutions that work in a 200 sq ft apartment with 5 kids and no money for syringes. Maybe a community pharmacy program? Or free dosing tools at clinics?
Also - poison control number? We don’t even have that here. Just call the hospital and wait 3 hours. Not ideal.
Trevor Whipple 12.01.2026
Ugh. Another ‘you’re all bad parents’ article. I’m tired of being shamed for leaving a bottle on the counter. My kid is 18 months. He’s not a robot. He’s a human. He climbs. He grabs. He tastes. You think I don’t know this? I’ve been doing this for 18 months. I don’t need a 5000-word lecture on how I’m failing. I need someone to tell me how to do this when I’m sleep-deprived and my husband is working nights. And no, I can’t afford a $400 smart dispenser. I can barely afford diapers.
Also - ‘never use a spoon’? I used one for 6 months. My kid didn’t die. He’s fine. Maybe you’re overthinking this.
Lethabo Phalafala 12.01.2026
MY HEART IS BREAKING. I didn’t know any of this. I used a spoon. I left the bottle on the counter. I thought ‘it’s just a little bit’ - and then I read the part about infant drops being SIX TIMES stronger and I started crying in the grocery store. I have a 2-year-old. I’m terrified. I just went home and threw out all the old meds I was hoarding. I bought a lockbox. I saved poison control. I’m printing this out and taping it to my mirror. I don’t care if it’s overkill - I’d rather be paranoid than bury my child. Thank you. From the bottom of my soul - thank you.
Lance Nickie 12.01.2026
Spoons are fine. Just don’t be an idiot.
John Pope 12.01.2026
Let’s not pretend this is about safety. It’s about control. The pharmaceutical industry wants you to think your kid will die if you use a spoon - so you’ll buy their $500 ‘smart’ dispenser. They profit from fear. The real issue? We’ve medicalized parenting. Now every mistake is a potential tragedy. We’re raising a generation of kids who can’t even touch a pill without a 12-step protocol.
Also - why is naloxone for kids even a thing? Are we prescribing opioids to toddlers now? That’s the real problem. Fix the prescribing culture, not the storage. And don’t tell me to lock everything up. My kid is 2. He’s not a drug dealer. He’s a toddler. He wants candy. Give him candy. Don’t turn your home into a prison.
Angel Tiestos lopez 12.01.2026
✨ this post hit me in my soul. 🌱
i’ve been a parent for 3 years and i never knew infant drops were 6x stronger. i’ve used the wrong one. i’m so glad i didn’t lose my kid. 🥹
also - i saved poison control in my phone. i put it under ‘EMERGENCY’ with a ❤️ emoji. i’m not ashamed. i’m empowered.
and the coffee grounds thing? genius. my cat hates it. so now she’s guarding the trash. bonus safety feature. 🐱💨
we’re not perfect. we’re human. but we can be better. thank you for not judging. just guiding. 🙏
Alan Lin 12.01.2026
This is a meticulously researched, evidence-based, and urgently necessary public health intervention. The data presented is not anecdotal - it is statistically significant, peer-reviewed, and actionable. The fact that 78.3% of dosing errors involve kitchen utensils is not a reflection of parental negligence, but of systemic failure in consumer education and product design. The PROTECT Initiative’s 25% reduction in ER visits is a testament to the power of coordinated, science-driven policy. I urge every healthcare provider, educator, and policymaker to adopt and amplify these protocols without delay. To dismiss this as ‘overkill’ is to misunderstand the stakes. One child’s life is not a statistical outlier - it is an irreplaceable human being. This is not about fear. It is about responsibility. And responsibility is non-negotiable.
Priyanka Kumari 12.01.2026
Thank you for this. I’m a nurse in India and I see this every day - parents giving adult doses because they don’t know the difference. I’ve started handing out free dosing syringes at clinics. I print out the poison control number in Hindi and Tamil and give it to every parent. It’s small, but it helps. I also tell them: ‘Your child doesn’t need perfection. They need you to be consistent.’ One locked cabinet. One syringe. One saved number. That’s enough. You’re not failing. You’re learning. And you’re not alone.
Avneet Singh 12.01.2026
Let’s be honest - this is just fearmongering dressed up as public health. The CDC’s ‘25% reduction’? That’s from 2010 to 2020. Meanwhile, ER visits for pediatric trauma from falls, burns, and car seats have skyrocketed - but no one’s writing 5000-word essays on ‘how to prevent your toddler from falling off the couch.’ Why? Because it’s not profitable. This whole ‘PROTECT’ campaign is a PR play to sell more child-resistant packaging and dosing tools. The real issue? Parental supervision. Not labels. Not syringes. Not locked cabinets. Just pay attention. It’s not rocket science. And if you can’t, maybe you shouldn’t be a parent.