Every year, thousands of people end up in the hospital not because their medicine didn’t work-but because something they ate, drank, or took as a supplement made it work too well, or not at all. It’s not rare. It’s not an accident. It’s a drug interaction, and it’s one of the most overlooked dangers in everyday health.
What Exactly Is a Drug Interaction?
A drug interaction happens when something changes how a medication behaves in your body. This could be food, another pill, a vitamin, or even a herbal supplement. The result? Your blood pressure might spike, your blood might not clot, your heart could race, or the drug might just vanish from your system without helping at all. There are three main types:- Drug-drug: Two medications interfere with each other.
- Drug-food: Something you eat or drink affects how the drug works.
- Drug-supplement: Vitamins, herbs, or minerals change the drug’s effect.
Grapefruit: The Silent Killer in Your Breakfast
Grapefruit is healthy. It’s full of vitamin C. It’s refreshing. But if you’re taking a statin like simvastatin or atorvastatin, it’s also dangerous. Grapefruit contains chemicals called furanocoumarins that shut down an enzyme in your gut called CYP3A4. This enzyme normally breaks down many drugs so they don’t build up too high in your blood. When it’s blocked, the drug stays in your system longer-and at much higher levels. One study found that drinking just one glass of grapefruit juice could increase simvastatin levels by up to 15 times. That’s not a typo. Fifteen times. Why does that matter? High statin levels can cause rhabdomyolysis-a condition where muscle tissue breaks down and floods your kidneys with toxic proteins. It can lead to kidney failure. The risk jumps from 0.15 cases per 100,000 people a year to 1.57 when grapefruit is involved. And it’s not just grapefruit. Pomelos, Seville oranges, and some tangelos do the same thing. If you’re on a statin, skip them entirely. Even a single glass can have effects lasting over 24 hours.Warfarin and Leafy Greens: A Dangerous Balance
Warfarin is a blood thinner. It keeps clots from forming-critical for people with atrial fibrillation, artificial heart valves, or a history of strokes. But warfarin works by blocking vitamin K, which your body needs to make clotting factors. So if you suddenly eat a lot of vitamin K-rich foods-like spinach, kale, broccoli, or Brussels sprouts-you’re fighting the drug’s purpose. A 2018 study showed that eating 150 grams of cooked spinach (about a cup and a half) could cut warfarin’s effect by 30-40% in less than a day. Your INR-a measure of how long your blood takes to clot-could drop dangerously low. That means you’re at risk of a stroke or pulmonary embolism. But here’s the twist: you don’t need to avoid these foods. You just need to keep them consistent. Eat the same amount every day. If you usually eat a salad once a week, keep doing that. Don’t suddenly start eating three cups of kale every morning. The FDA recommends 90 mcg of vitamin K daily for women and 120 mcg for men. That’s about one serving of leafy greens. Stick to it.St. John’s Wort: The Supplement That Can Kill Your Medication
St. John’s wort is sold as a natural remedy for mild depression. It’s widely available. It’s cheap. And it’s one of the most dangerous supplements you can take with prescription drugs. It activates a liver enzyme called CYP3A4-exactly the opposite of grapefruit. Instead of blocking drug breakdown, it speeds it up. That means your medication gets flushed out of your system too fast. Take cyclosporine (used after organ transplants)? St. John’s wort can drop its levels by 50-70% in two weeks. Your body might reject the new organ. On birth control? The risk of unintended pregnancy jumps by 50-70%. That’s not a guess. That’s from clinical studies. On an SSRI like sertraline or fluoxetine? You could develop serotonin syndrome-a medical emergency. Symptoms: high fever, muscle stiffness, confusion, rapid heartbeat, seizures. It can kill you in hours. And it doesn’t stop there. St. John’s wort also messes with HIV meds, cancer drugs, and even some heart medications. Over 50% of prescription drugs are affected. The FDA doesn’t require warning labels on supplements. So unless you read the fine print or ask your pharmacist, you won’t know.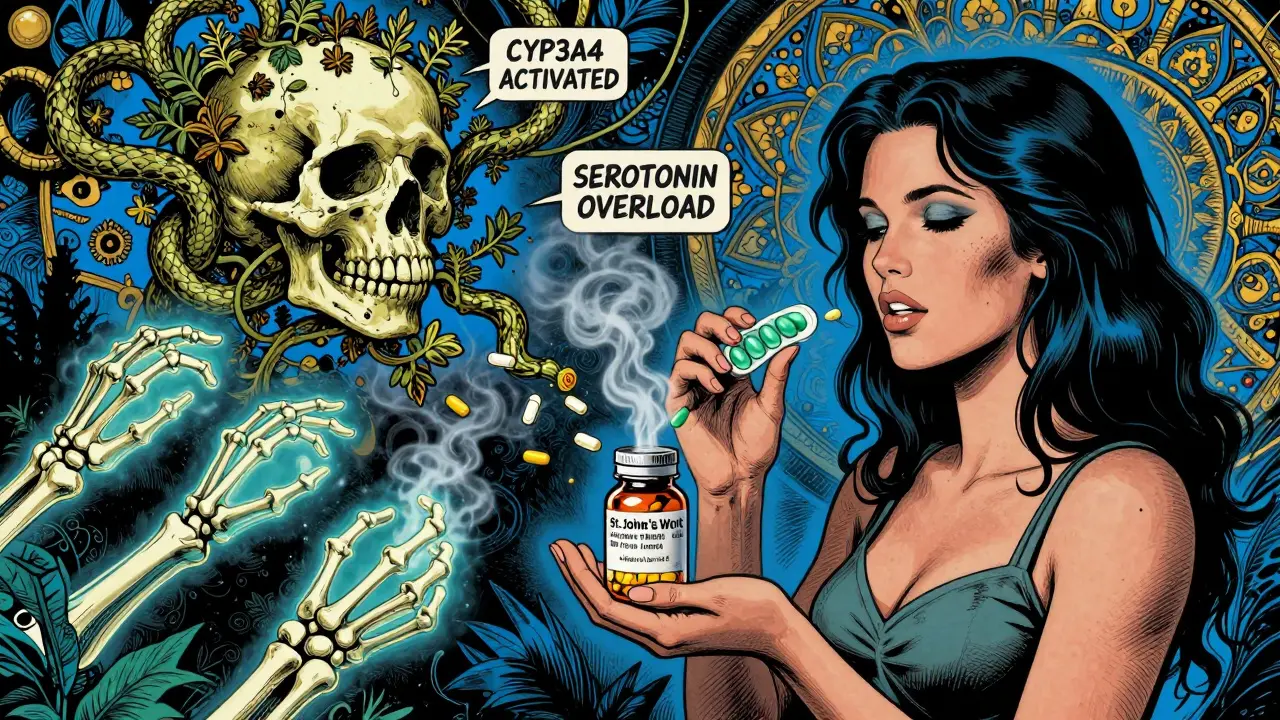
Ginkgo, Garlic, and the Bleeding Risk
Ginkgo biloba is used for memory and circulation. Garlic is for heart health. Both sound harmless. But together with blood thinners like warfarin, aspirin, or clopidogrel? They’re a recipe for bleeding. Ginkgo blocks platelet activation. That means your blood can’t clot as easily. Studies show it can increase bleeding time by 30-50%. In one case, a man on warfarin took ginkgo and ended up with a brain bleed. Garlic supplements? A 2001 study found 32 documented cases of dangerous bleeding when garlic was taken with warfarin, heparin, or aspirin. Some patients needed emergency transfusions. Even fish oil-often recommended for heart health-can thin the blood. If you’re on anticoagulants, your doctor needs to know if you’re taking more than 3 grams of omega-3s a day.Red Yeast Rice: A Natural Statin With a Hidden Cost
Red yeast rice is marketed as a “natural” way to lower cholesterol. It sounds safe. But it contains monacolin K-the exact same compound as lovastatin, a prescription statin. If you’re already taking a statin like atorvastatin or rosuvastatin and add red yeast rice? You’re doubling your statin dose. That’s not natural. That’s risky. A 2017 study found this combo increased the risk of muscle damage (myopathy) by 2.3 times. Some people developed rhabdomyolysis. And here’s the kicker: red yeast rice isn’t regulated like a drug. So you don’t know how much monacolin K is in each pill. One brand might have 5 mg. Another might have 15 mg. No one’s checking.What You Can Do Right Now
You don’t need to stop taking supplements. You don’t need to give up your favorite foods. But you do need to be smart. Here’s what works:- Keep a full list of everything you take: prescription drugs, over-the-counter meds, vitamins, herbs, teas, and even CBD or melatonin. Update it every time you see a doctor or pharmacist.
- Ask your pharmacist every time you pick up a new prescription. Pharmacists are trained to spot interactions. They check for them daily. Use that resource.
- Use free tools like MedlinePlus Drug Interaction Checker. Type in your meds and supplements. It’s free, reliable, and updated regularly.
- Don’t assume “natural” means safe. Just because it’s sold in a health food store doesn’t mean it won’t harm you.
- Tell your doctor about supplements. Studies show 70% of people don’t mention them. That’s not because they’re hiding-it’s because they don’t think it matters. It does.


LIZETH DE PACHECO 31.12.2025
I used to take St. John’s Wort with my antidepressant because I thought 'natural' meant safe. Turns out I almost ended up in the ER. My doctor didn’t even ask about supplements. Never again. Talk to your pharmacist. Seriously.
Also, grapefruit juice is now banned from my kitchen. No regrets.
Lee M 31.12.2025
So let me get this straight-you’re telling me the entire supplement industry is a scam run by wellness influencers who don’t know biochemistry? Of course it is. The FDA doesn’t regulate supplements because they’re too busy protecting Big Pharma’s profits. Wake up. Natural doesn’t mean harmless-it means unregulated. And that’s the point.
Matthew Hekmatniaz 31.12.2025
I grew up in a family where everything was 'natural'-turmeric for everything, garlic pills for blood pressure, ginkgo for memory. We didn’t know any better. Now I’m the one reminding my mom that her 'miracle tea' could mess with her blood thinner. It’s not about fear. It’s about awareness. Education saves lives, not just pills.
Also, I’m glad the FDA’s finally pushing for labeling. Took them long enough.
Dusty Weeks 31.12.2025
st johns wort is literally a drug bro why are people still taking it like its a tea 🤡
also grapefruit juice? dude its not a smoothie ingredient its a pharmacy hazard
and red yeast rice? that's just statin in disguise. why are we still doing this? 🤦♂️
Paul Ong 31.12.2025
Just started taking warfarin last month. My doctor said eat your greens but keep it consistent. I’ve been having one cup of spinach every morning. No more surprises. Simple. Smart. Done.
Also-pharmacists are your real heroes. Never skip asking them.
Austin Mac-Anabraba 31.12.2025
It’s not that people are ignorant-it’s that they’re willfully negligent. You don’t get to cherry-pick science because it’s convenient. St. John’s Wort isn’t 'alternative medicine'-it’s a CYP3A4 inducer with documented, life-threatening interactions. If you’re taking it with SSRIs, you’re playing Russian roulette with your serotonin levels. The fact that this is still common knowledge among the public is a national embarrassment.
Phoebe McKenzie 31.12.2025
Of course you didn’t know grapefruit could kill you-you’re probably one of those people who thinks 'organic' means 'FDA approved.'
And don’t even get me started on red yeast rice. That’s not a supplement. That’s fraud. Someone’s making millions selling you a prescription drug in a bottle labeled 'herbal.'
Stop being gullible. Your life isn’t a TikTok trend.
gerard najera 31.12.2025
Food isn’t the enemy. Ignorance is.
Stephen Gikuma 31.12.2025
They don’t want you to know this. Why? Because if you knew how many drugs interact with your food, you’d stop trusting Big Pharma. Grapefruit? It’s not an accident. It’s a cover-up. The FDA lets supplements slide so they can control the narrative. You think they want you to be healthy? No-they want you dependent. Read between the lines.
Bobby Collins 31.12.2025
ok but what if the government is putting something in the grapefruit to make you sick?? like why would they let this be a thing??
also i heard ginkgo is made by the illuminati to control your brain
why do they care if you take supplements??
they dont want you to be healthy they want you to be a patient
ask yourself why
Layla Anna 31.12.2025
I’m 28 and on birth control. I took St. John’s Wort for a month because I was stressed. Didn’t think it mattered. Got pregnant.
Now I tell everyone. Please. Just check before you take anything. Even if it’s 'just a herb.'
I’m so lucky I didn’t lose my life over it.
Thank you for writing this. ❤️
sharad vyas 31.12.2025
In India, many people use turmeric with blood thinners. No one tells them. I told my uncle. He stopped. He is fine now. Small things matter. Thank you for sharing.
Bill Medley 31.12.2025
While the article presents compelling clinical evidence, it is imperative to emphasize that patient autonomy must be balanced with professional guidance. The onus of pharmacovigilance should not rest solely upon the layperson; regulatory bodies, healthcare institutions, and pharmaceutical manufacturers share collective responsibility for transparent communication and standardized labeling protocols. The current landscape is not merely inadequate-it is ethically indefensible.