Epidural Hematoma Risk Calculator
Recommended Actions
Important Safety Information
Remember: Do not stop your anticoagulants without consulting your doctor. Stopping medications like warfarin or LMWH without proper guidance can cause serious complications like stroke or pulmonary embolism.
Getting an epidural or spinal injection while on blood thinners sounds simple-until something goes wrong. For many patients, especially older adults or those with heart conditions, these procedures are necessary for pain relief or surgery. But when you’re taking warfarin, enoxaparin, rivaroxaban, or any other anticoagulant, the risk of a rare but devastating complication-epidural hematoma-goes up. And it doesn’t take much: as little as 1-2 mL of blood in the wrong spot can crush your spinal cord.
What Exactly Is an Epidural Hematoma?
An epidural hematoma happens when blood leaks into the space between the dura (the tough outer membrane around your spinal cord) and the ligamentum flavum (a ligament in your spine). This space is tiny, so even a small amount of bleeding creates pressure. That pressure can squeeze your spinal cord, cutting off nerve signals. Symptoms come fast: severe back pain, numbness in your legs, weakness, or trouble peeing or pooping. If you feel any of these within hours after a spinal procedure, it’s an emergency.Studies show 93% of patients with this complication report midline back pain first. Around 76% develop leg weakness. And if treatment is delayed past 24 hours, only 9% recover fully. But if you get surgery within 8 hours, that jumps to 79%. Time isn’t just important-it’s everything.
Which Blood Thinners Are Most Dangerous?
Not all anticoagulants carry the same risk. Here’s how they stack up:- Warfarin: Risk spikes when INR (a blood clotting test) is above 1.4. At that level, your chance of hematoma jumps 8.7 times compared to normal. Even if your INR is back to normal before the procedure, there are documented cases of hematomas anyway.
- Low Molecular Weight Heparin (LMWH) (like Lovenox): Therapeutic doses (used for clots) are far riskier than prophylactic doses (used to prevent clots). If you get a shot within 8 hours of the procedure, your risk is 0.31%. Wait 24 hours, and it drops to 0.04%.
- DOACs (rivaroxaban, apixaban, dabigatran, edoxaban): These newer drugs are popular because they don’t need blood tests. But timing matters. For rivaroxaban, stopping 48 hours before a procedure keeps risk at 0.08%. Stop too late, and it jumps to 0.42%. Apixaban is slightly safer, with a 0.05% risk when timed right. But there are cases-even with 72 hours of stopping-where hematomas still happened.
- Antiplatelets (aspirin, clopidogrel): Aspirin alone? Risk is nearly negligible (0.03%). But if you’re on both aspirin and clopidogrel? Risk triples. Many doctors now advise stopping dual therapy 7 days before a spinal procedure.
The FDA reviewed over 170 cases tied to Lovenox alone between 1992 and 2013. That’s why they now require specific warnings on all anticoagulant labels. It’s not theoretical-it’s happened, and often.
Who’s at Highest Risk?
It’s not just about the drug. Your body matters too. Here are the biggest red flags:- Age over 70: Your blood vessels become more fragile. Risk jumps 3.7 times.
- Kidney problems (CrCl under 30 mL/min): Your body can’t clear drugs like rivaroxaban or apixaban properly. Risk increases nearly 5 times.
- Spinal stenosis: A narrowed spine leaves less room for blood to spread. Even small clots cause big damage. Risk: 2.8 times higher.
- Multiple needle attempts: If the anesthesiologist has to poke more than twice, your risk jumps 6.2 times.
- Blood-tinged fluid: If they see blood when they draw spinal fluid, your risk goes up 11.8 times.
- Epidural catheter: Leaving a tube in place (instead of one shot) increases risk 2.3 times.
- Low hemoglobin (under 10 g/dL): Your body is already struggling to carry oxygen. Add bleeding? Danger multiplies.
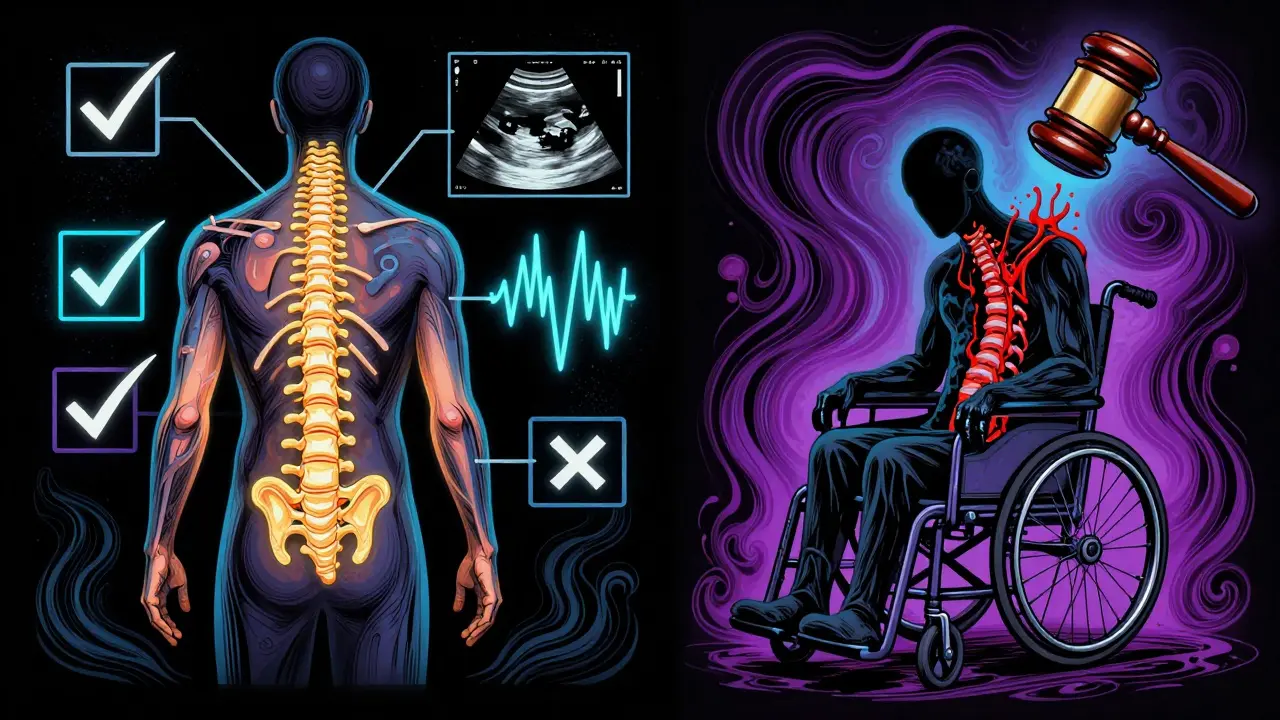
One study of over 12,000 spinal procedures found that patients with three or more of these factors had a 1 in 100 chance of developing a hematoma. That’s not rare. That’s a real, measurable threat.
When Should You Stop Your Blood Thinners?
Timing isn’t guesswork. It’s science. Here’s what the latest guidelines say:- Warfarin: Check INR within 24 hours before the procedure. Target: under 1.4. Restart 4 hours after a single shot, 6 hours after a catheter.
- LMWH (prophylactic dose): Stop 10-12 hours before. For therapeutic dose: stop 24 hours before. Restart 2 hours after single shot, 4 hours after catheter.
- Rivaroxaban, apixaban: Stop 48 hours before if kidneys are normal. If kidney function is poor, stop 72 hours before. Restart 2-4 hours after procedure, depending on catheter use.
- Dabigatran: Stop 48 hours before normal kidney function; 72 hours if impaired.
- Aspirin: Can usually stay on. No need to stop.
- Clopidogrel: Stop 7 days before if possible, especially if combined with aspirin.
Here’s the catch: a 2022 survey found only 58% of pain doctors knew the correct timing for DOACs. And 27% admitted to a near-miss because of a timing error. That’s not because they’re careless-it’s because the rules are complex and change often.
What About Procedures Like Epidural Steroid Injections?
Not all spinal procedures are equal. A diagnostic lumbar puncture has a risk of just 0.001%. A single epidural steroid injection? About 1 in 15,000. But a spinal fusion? That’s up to 1%. And spinal cord stimulator placement? 0.14%-and of those who get a hematoma, one-third end up with permanent nerve damage.So if you’re getting a simple injection for back pain, the risk is very low-even on blood thinners-if guidelines are followed. But if you’re having major surgery, the stakes are much higher. Your doctor should weigh the pain relief against the risk of paralysis.
What Happens If a Hematoma Is Missed?
The consequences are brutal. Permanent paraplegia happens in 24% of cases. About 3-5% of patients die if treatment is delayed. The average cost of managing one case? Nearly $288,000. That includes surgery, months of rehab, and lifelong care.And it’s not just medical-it’s legal. In 2022, there were 78 malpractice claims in the U.S. tied to these hematomas. Sixty-two percent ended in settlements, averaging $1.2 million. The most common reason? Failure to follow timing guidelines. The second? Not checking for symptoms after the procedure.
What’s Changing in 2025?
New tools are coming. The FDA now requires all anticoagulant manufacturers to run education programs for prescribers. Hospitals performing over 50 spinal procedures a year must report hematoma rates starting January 2025. And researchers are testing blood markers-like GFAP levels-that can detect a developing hematoma within 2 hours of the procedure, long before symptoms show.Also, new guidelines expected in 2024 will use a scoring system. You’ll get points for age, kidney function, drug type, number of needle passes, and more. A score over 15? You’re high risk. That means no spinal block. Maybe an alternative pain method, like a nerve block or oral meds.
One surprising finding? Women appear to be 2.3 times more likely to develop a hematoma than men-even when on the same drugs, same doses. Why? No one knows yet. But it’s being studied.
What Should You Do?
If you’re on blood thinners and scheduled for a spinal procedure:- Bring a full list of all your medications-including over-the-counter aspirin or fish oil.
- Ask: “What’s my risk for a hematoma based on my drugs and health?”
- Ask: “What’s the plan if I develop pain or numbness after the procedure?”
- Ask: “Will you check my INR or kidney function before?”
- Ask: “Can you use ultrasound to guide the needle? That reduces multiple attempts.”
Don’t assume your doctor knows the latest guidelines. Many don’t. And don’t stop your meds on your own. Stopping warfarin or LMWH without backup can trigger a stroke or pulmonary embolism. The goal isn’t to avoid all risk-it’s to balance it.


Ed Di Cristofaro 31.01.2026
People still don’t get it. You don’t just ‘stop your blood thinners’ like you’re turning off a faucet. I had my dad nearly die because his nurse ‘assumed’ his INR was fine. It wasn’t. He got the shot anyway. Now he’s in a wheelchair. Don’t be that guy. Know your numbers. Ask twice. Write it down. This isn’t a suggestion-it’s a life-or-death checklist.