Head Injury Risk Assessment
Assess Your Situation
This tool helps you determine if you need immediate medical attention after a head injury while on blood thinners.
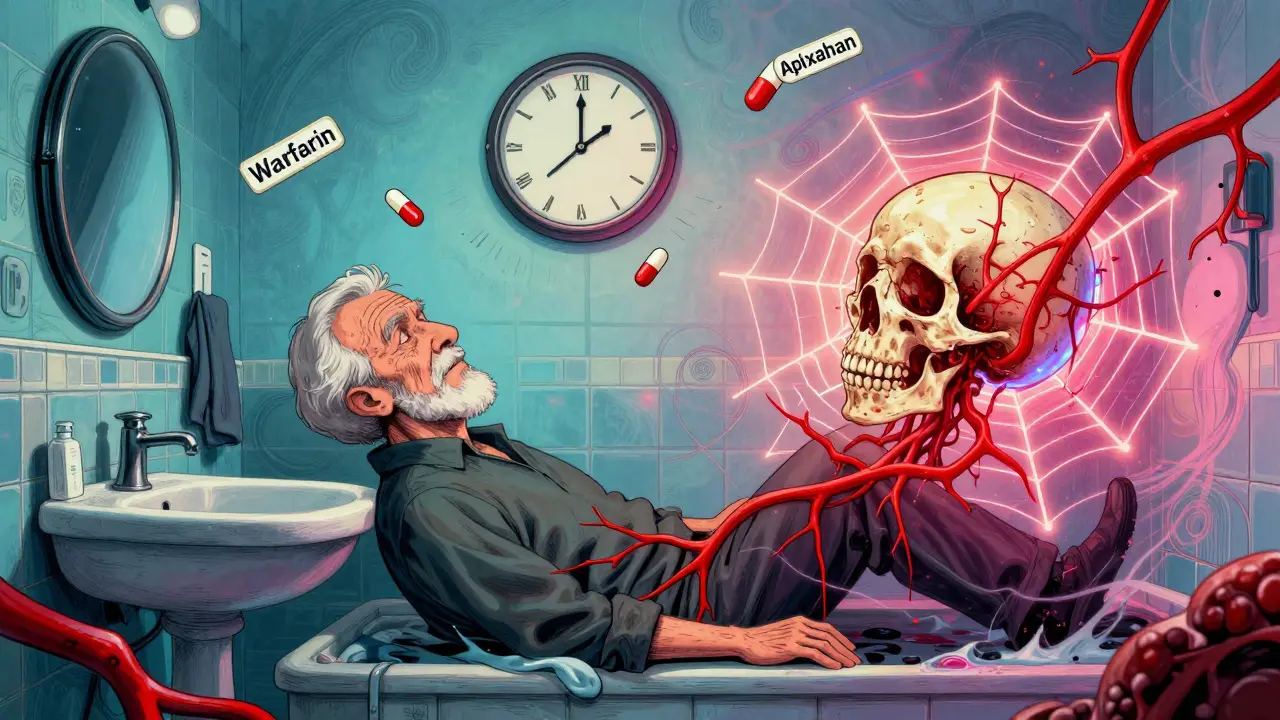
If you’re on blood thinners and you hit your head-even lightly-you can’t just brush it off. That minor bump could turn into a life-threatening bleed inside your skull, and you won’t necessarily feel it coming. Unlike someone not on anticoagulants, your body doesn’t stop bleeding the same way. A fall from standing height, a slip on the bathroom floor, or even a bump from a doorframe can be enough to trigger a dangerous bleed. The clock starts ticking the moment you’re injured, and waiting too long to get checked can cost you your life.
Why Blood Thinners Change Everything After a Head Injury
Blood thinners like warfarin, rivaroxaban, apixaban, and dabigatran are prescribed to prevent clots in people with atrial fibrillation, deep vein thrombosis, or artificial heart valves. But they also make your blood less able to clot when you’re injured. After a head injury, your brain can bleed internally even if there’s no visible cut, bruise, or loss of consciousness. Studies show people on these medications have 2 to 3 times higher risk of intracranial hemorrhage after even minor trauma compared to those not on blood thinners.
This isn’t theoretical. In emergency rooms across the U.S. and Australia, about 1 in 10 head injury cases involve someone on anticoagulants. And while many of these patients feel fine at first, delayed bleeding can happen-sometimes hours or even days later. One study found that 0.5% to 1% of anticoagulated patients with a normal initial CT scan developed a bleed within 72 hours. That’s why the standard advice isn’t “wait and see.” It’s “get scanned now.”
When to Go Straight to the ER
You don’t need to wait for symptoms to get worse. If you’re on blood thinners and you’ve had any kind of head impact, you should go to the emergency department immediately if you have:
- Any loss of consciousness-even for a few seconds
- Confusion, dizziness, or trouble remembering what happened
- Headache that gets worse over time
- Nausea or vomiting (especially more than once)
- Blurred vision, slurred speech, or weakness on one side of the body
- A fall from standing height or higher, especially if you’re over 65
- Any sign of injury to the head or neck-bruising, swelling, or deformity
Even if you’re not sure, it’s better to be safe. Emergency guidelines from the American College of Emergency Physicians (ACEP) and the Washington State Department of Health both say: any adult on anticoagulants with head trauma should get a CT scan right away. No exceptions. No waiting. No “let’s see how you feel in an hour.”
What Happens in the Emergency Room
When you arrive, you’ll be fast-tracked. Emergency staff know that for anticoagulated patients, every minute counts. You’ll likely get two things immediately: a blood test and a CT scan.
The blood test checks your clotting status. For warfarin users, they’ll look at your INR (International Normalized Ratio). If it’s above 3.5, your risk of bleeding is much higher. For newer drugs like rivaroxaban or apixaban, they’ll check when you last took your dose and may order a specific blood test to measure drug levels.
The CT scan is non-contrast, meaning no dye is used. It’s fast, accurate, and designed to catch even tiny bleeds. Radiologists use high-resolution “bone algorithm” images to spot skull fractures that might not show up on a regular scan. The scan results are reviewed by a radiologist immediately, and the doctor treating you gets the findings within minutes.
Some hospitals also check for brain injury biomarkers like GFAP and UCH-L1. These proteins leak into the blood when brain cells are damaged. While not yet standard everywhere, they’re becoming more common in trauma centers and can help avoid unnecessary scans in low-risk patients-though they’re still not recommended for those on blood thinners.

What If the CT Scan Is Normal?
A normal CT scan doesn’t mean you’re in the clear. Bleeding can still develop hours later. That’s why observation is critical.
Most guidelines recommend a 6-hour observation period after the injury, during which you’re monitored for changes in alertness, speech, movement, or pain. If you stay stable, your INR is under control, and you have no other injuries, you might be discharged with clear instructions.
But here’s what you need to know: you must watch for warning signs after you go home. If you develop any of these within the next 48 hours, go back to the ER immediately:
- Worsening headache
- Repeated vomiting
- Difficulty waking up or staying awake
- Seizures
- Weakness in an arm or leg
- Slurred speech or confusion
- Unequal pupil size
Even if you feel fine, don’t stop taking your blood thinner unless a doctor tells you to. Stopping it suddenly can trigger a stroke or blood clot. One patient in a major study stopped rivaroxaban after a negative CT scan-and had a stroke three days later. The risk of clotting can be just as deadly as bleeding.
When You Might Need a Second Scan
Not everyone needs a repeat CT. The ACEP says you don’t need to repeat the scan if you’re feeling your normal self, your INR is stable, and you had no bleeding on the first scan. But some hospitals still do a second scan after 6-24 hours, especially for older patients or those on stronger anticoagulants.
At the University of Texas, patients are kept for 23 hours and get a second scan if they have any of these:
- Age over 65
- INR over 3.5
- History of alcohol abuse
- Any sign of neurological change during observation
Johns Hopkins and other top trauma centers have adopted 24-hour observation for all anticoagulated patients, regardless of initial scan results. Why? Because delayed bleeding doesn’t follow a schedule. It happens when it wants to.
What You Can Do Before You Get Hurt
Prevention is your best defense. If you’re on blood thinners, you’re at higher risk for falls. Talk to your doctor about:
- Removing tripping hazards at home (rugs, clutter, poor lighting)
- Installing grab bars in the bathroom
- Wearing non-slip shoes
- Reviewing your medications for dizziness side effects
- Getting your vision checked regularly
Some clinics now use the CDC’s STEADI program to assess fall risk and balance in older adults on anticoagulants. It’s not just about preventing clots-it’s about preventing the injuries that can make those clots deadly.

What Doctors Wish You Knew
Emergency physicians see this too often. A patient comes in after a fall, says, “I didn’t think it was serious,” and then has a bleed that could’ve been caught early. Here’s what they want you to remember:
- There’s no such thing as a “minor” head injury when you’re on blood thinners.
- Waiting for symptoms to appear is dangerous. Bleeding doesn’t always hurt right away.
- CT scans are quick, safe, and worth it. The radiation risk is tiny compared to the risk of a brain bleed.
- Don’t stop your blood thinner without talking to your doctor-even if you think it’s safer.
- Have someone with you when you go to the ER. You might not remember everything the doctor says.
One doctor put it simply: “If you’re on a blood thinner and you hit your head, you’re not just having a head injury. You’re having a medical emergency. Treat it like one.”
What Happens If Bleeding Is Found?
If the CT shows a bleed, your care team will act fast. Depending on the size and location, you might need:
- Reversal agents like Idarucizumab (for dabigatran) or Andexanet alfa (for rivaroxaban/apixaban)
- Prothrombin complex concentrate (PCC) for warfarin
- Blood transfusions
- Neurosurgery to relieve pressure on the brain
Reversal agents can stop the bleeding in minutes. But they’re not magic-they only work if given quickly. That’s why getting to the hospital fast matters more than you think.
After the bleed is controlled, your doctor will decide whether to restart your blood thinner. That decision balances the risk of another bleed against the risk of a stroke or clot. It’s never a simple yes or no. It’s a conversation-with your neurologist, cardiologist, and primary care doctor.
Do I need a CT scan if I hit my head and feel fine?
Yes. If you’re on blood thinners, even a small bump can cause internal bleeding that doesn’t cause symptoms right away. Guidelines from the American College of Emergency Physicians and Washington State Health Department recommend an immediate CT scan for any head injury in anticoagulated patients, regardless of how you feel. Waiting for symptoms can be deadly.
Can I wait a few hours to see if I feel worse?
No. Delaying imaging increases your risk of complications. Studies show that brain bleeds can grow rapidly in people on anticoagulants. Emergency departments prioritize these patients because every minute counts. The goal is to catch bleeding before it causes permanent damage or becomes life-threatening.
Is a CT scan safe for someone on blood thinners?
Yes. A non-contrast head CT uses minimal radiation and carries no risk of bleeding from the scan itself. The benefit of detecting a brain bleed far outweighs the tiny radiation exposure. Not getting scanned is the real danger.
What if my INR is normal? Do I still need a scan?
Yes. Even if your INR is in range, your blood is still thinner than normal. The risk of bleeding after trauma doesn’t disappear just because your lab numbers look good. The mechanism of injury matters more than your current INR. A fall from standing height is enough to trigger a bleed, regardless of lab values.
Can I go home if the CT scan is normal?
Maybe-but only after a 6-hour observation period and if you meet specific safety criteria: no neurological changes, stable INR (under 3.5 for warfarin), and no other injuries. You’ll get detailed instructions on warning signs to watch for. If you develop any new symptoms, return to the ER immediately.
Should I stop taking my blood thinner after a head injury?
Never stop without talking to your doctor. Stopping your blood thinner can cause a stroke or clot, which can be just as deadly as a brain bleed. One patient stopped rivaroxaban after a negative CT scan and had a stroke three days later. Your care team will weigh the risks of bleeding versus clotting before making any changes.
How long should I be monitored after a head injury?
At least 6 hours in the hospital, even if the CT is normal. Some hospitals keep patients for 24 hours, especially if they’re over 65 or on stronger anticoagulants. Bleeding can develop up to 72 hours after the injury, so you need to be watched closely and know the warning signs.
Are there alternatives to CT scans for anticoagulated patients?
MRI is more sensitive for some types of brain injury and avoids radiation, but it’s not used for initial evaluation because it takes longer and isn’t always available in emergencies. Blood biomarkers like GFAP are being studied, but they’re not yet reliable enough to replace CT scans in anticoagulated patients. CT remains the gold standard for fast, accurate diagnosis.
Next Steps After a Head Injury
If you’ve been cleared to go home:
- Have someone stay with you for at least 24 hours.
- Check in with your doctor within 24-48 hours.
- Keep your scheduled blood tests (INR, drug levels) as directed.
- Don’t drink alcohol or take NSAIDs like ibuprofen-they can increase bleeding risk.
- Write down the warning signs and keep them where you can see them.
If you’re still in the hospital, ask your care team: “What’s my plan if I feel worse tonight?” and “When will I get my next scan?” Don’t assume someone else is watching. Be your own advocate.
Head injuries on blood thinners are serious-but they’re preventable if you act fast. Knowing when to go to the ER could save your life. Don’t wait. Don’t guess. Get scanned.

Jacob Paterson 7.01.2026
Oh wow, another ‘just go to the ER’ checklist. Because clearly, the only solution to life is infinite hospital visits. I hit my head on a cabinet last week-no CT, no drama. Guess I’m just lucky my blood isn’t ‘thinned’ by the government’s pharmaceutical agenda.
Angela Stanton 7.01.2026
Let’s break this down with some clinical nuance: anticoagulant-associated ICH has a biphasic risk curve-initial surge post-trauma, then delayed peak at 24–48h. The ACEP guidelines are *mostly* evidence-based, but the 100% CT mandate ignores cost-effectiveness thresholds (ICER >$150k/QALY in low-risk subgroups). Also, GFAP/UCH-L1 biomarkers are now validated in Level 1 trauma centers-why are we still doing 300+ CTs per 100 patients? The algorithm needs recalibration.
Alicia Hasö 7.01.2026
THIS. IS. CRUCIAL. 🙌 If you’re on blood thinners, your body doesn’t get a ‘pass’ because you ‘felt fine.’ I watched my mom go from a simple bathroom slip to brain surgery in 14 hours-all because she waited to ‘see if it got worse.’ Don’t be her. Get scanned. No excuses. Your life isn’t a gamble. The scan takes 5 minutes. The recovery from a bleed? Months. Or forever. Don’t wait. Just go.
Ashley Kronenwetter 7.01.2026
While the clinical recommendations are sound, it is important to acknowledge that access to emergency imaging remains inequitable across socioeconomic and geographic lines. For patients without transportation, insurance, or proximity to trauma centers, the directive to ‘go immediately’ may be impractical. Systemic solutions are needed alongside individual education.
Heather Wilson 7.01.2026
Wow, this post is basically a 2000-word fear campaign. Let me guess-you work for a radiology startup? Or maybe you’re just terrified of your own shadow. I’ve been on warfarin for 8 years. I’ve fallen three times. No CTs. No bleeds. The real danger is overmedicalization. Your INR is normal? You’re fine. Stop panic-buying MRIs.
Also, why does every single sentence end like a PSA? ‘Get scanned now.’ ‘Don’t wait.’ ‘It could kill you.’ I get it. You’re scared. But not everyone needs a crisis every time they stub their toe.
Jeffrey Hu 7.01.2026
Actually, you’re all missing the point. The real issue isn’t the CT scan-it’s the reversal agents. Most ERs don’t stock Andexanet alfa because it costs $40k per dose. So even if you get scanned, if you’re on apixaban and bleed out, you’re basically screwed unless you’re in a Level 1 trauma center. And guess who can’t afford that? Everyone outside of Manhattan. So the real advice? Don’t fall. Ever. And if you do? Hope you live near a hospital with a $100M neurosurgery budget.
Drew Pearlman 7.01.2026
I just want to say how proud I am of you for sharing this. It takes courage to talk about something so scary, and honestly? You’re helping people feel less alone. I know it’s easy to feel like you’re overreacting after a little bump, but you’re not. You’re being responsible. And that’s something to celebrate. Even if you never need a scan again, just knowing this info could save your life-or someone else’s. Keep spreading awareness. You’re doing amazing work.
Meghan Hammack 7.01.2026
My dad’s on rivaroxaban. He fell last winter. We went straight to ER. CT was clear. They kept him overnight. Turned out he had a tiny bleed that showed up on the second scan. He’s fine now. But if we’d waited? He wouldn’t be. So listen: if you’re on blood thinners and you hit your head? Go. Now. No ‘maybe.’ No ‘I’ll wait.’ Just go. Your brain doesn’t care how ‘minor’ it feels. Neither should you.
RAJAT KD 7.01.2026
Correct. Delayed intracranial hemorrhage in anticoagulated patients is well-documented. Even minor trauma requires imaging. This is not optional. It is standard of care. Do not delay.
Matthew Maxwell 7.01.2026
Let me be blunt: anyone who reads this and still thinks they can ‘wait and see’ is either dangerously naive or actively endangering their life. This isn’t a suggestion. It’s a medical imperative. The fact that people even ask ‘Do I need a scan if I feel fine?’ proves we’ve failed as a society to teach basic risk awareness. If you’re on anticoagulants, you are not ‘normal.’ You are a walking time bomb. And ignorance is not a valid excuse for ignoring the most basic safety protocol in modern medicine. Get scanned. Or don’t. But don’t come crying to me when you’re brain-dead.