Keeping a list of your medications is important. But just listing pills and doses isn’t enough. If you’re taking high-risk drugs like insulin, opioids, blood thinners, or chemotherapy agents, you need to document safety alerts right on that list. These aren’t just reminders-they’re life-saving notes that prevent deadly mistakes.
Why Safety Alerts on Your Medication List Matter
Not all medications are created equal. Some, called high-alert medications, can cause serious harm-even death-if taken incorrectly. The Institute for Safe Medication Practices (ISMP) lists 19 categories of these drugs, including insulin, morphine, heparin, and neuromuscular blockers. A simple error-like taking daily methotrexate instead of weekly-can lead to organ failure. In hospitals, proper documentation of safety alerts has been shown to cut medication errors by up to 50%. But this isn’t just for hospitals. At home, a clear, visible alert on your personal medication list can stop a family member or pharmacist from making a fatal mistake.What Counts as a Safety Alert?
A safety alert isn’t just “Take with food.” It’s a specific, urgent warning tied to a known risk. Here’s what to include:- Insulin: “WARNING: Do not use if cloudy or clumped. Always verify type and dose before injection.”
- Warfarin or other anticoagulants: “HIGH RISK: Bleeding risk. Do not start new OTC meds (like ibuprofen) without doctor approval.”
- Oral methotrexate: “FOR WEEKLY USE ONLY. Daily use can be fatal.”
- Opioids: “RISK OF RESPIRATORY DEPRESSION. Do not mix with alcohol or sleep aids.”
- Neuromuscular blockers (rare at home, but possible post-surgery): “CAUSES PARALYSIS. Requires ventilator support.”
These aren’t opinions. They come from official sources: ISMP guidelines, FDA MedWatch alerts, and drug manufacturer safety communications. If your doctor prescribes one of these, ask them to write the exact safety phrase on your list. Don’t rely on memory.
How to Document Alerts on Your List
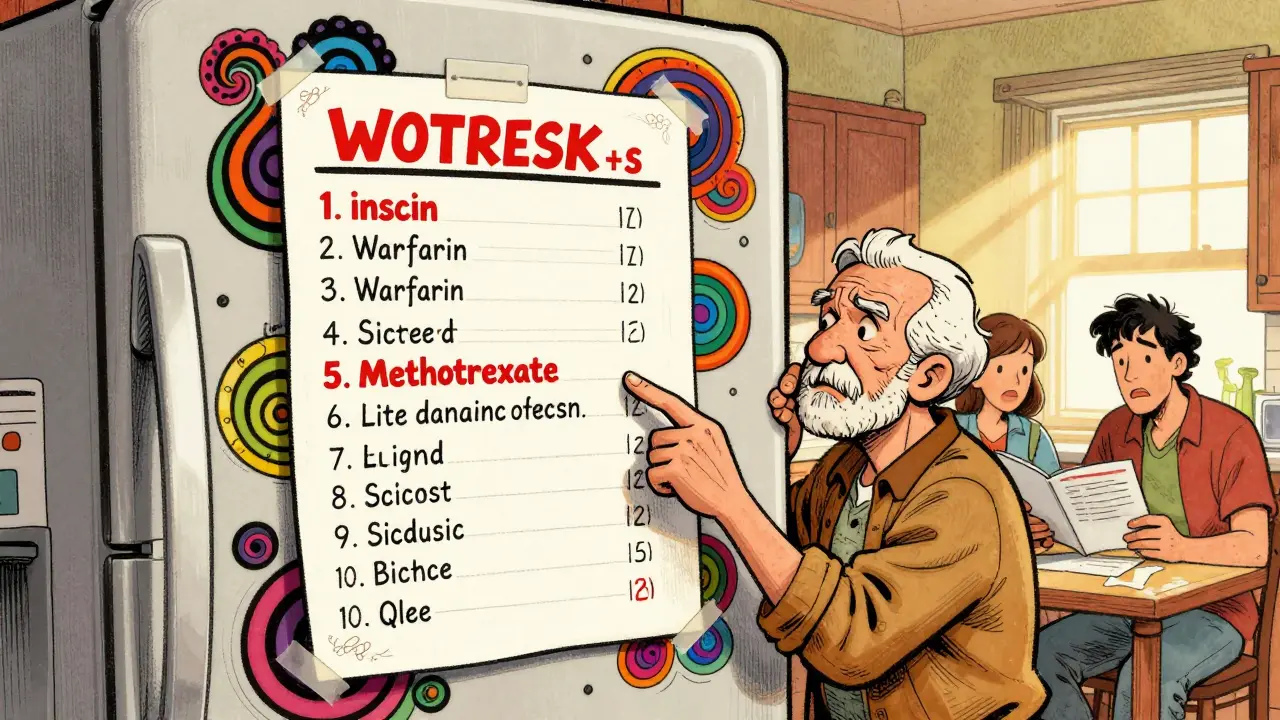
Start with a simple, physical or digital list. But don’t just write it in small print. Make it impossible to miss.- Use red text or a highlighter for all safety alerts. Color stands out better than bold.
- Place alerts directly next to the drug name, not at the bottom of the page.
- Include the reason. Don’t just say “High risk.” Say “High risk: Can cause low blood sugar if skipped or overdosed.”
- Update every time your regimen changes. A new alert means rewriting the list. Don’t scribble over old text.
- Share it with your pharmacist, caregiver, and family. If you’re hospitalized, hand them a printed copy. Ask them to verify the alerts are there.
Many people use apps like MyTherapy or Apple Health to track meds. That’s fine-but check if they allow you to add custom safety alerts. Most don’t. If yours doesn’t, print a paper copy and keep it in your wallet or on your fridge.
Common Mistakes to Avoid
Even well-meaning people mess this up.- Writing vague alerts: “Be careful with this drug” isn’t helpful. Be specific.
- Ignoring new alerts: The FDA issues about 120 drug safety updates a year. If your medication gets a new warning, update your list immediately.
- Only documenting for yourself: If you live alone or have memory issues, your alert list is useless if no one else knows it exists.
- Assuming your doctor wrote it: Doctors are busy. They may not write the alert on your list. You have to ask.
One patient in Sydney, 72, took daily methotrexate for rheumatoid arthritis for three years. Her doctor never told her it was meant to be weekly. Her list had no alert. She ended up in the ER with bone marrow failure. A simple, red-alert note could have prevented it.
What to Do If You Can’t Get an Alert Added
Sometimes, doctors or pharmacies say, “We don’t do that.” Don’t accept that.- Ask for a printed copy of the ISMP safety guideline for your drug. Print it from ismp.org.
- Take it to your pharmacist and say: “This is the official warning. Can you add it to my profile?”
- If they refuse, ask to speak to the pharmacy’s medication safety officer. Every major pharmacy has one.
- Write it on a sticky note and tape it to your pill bottle.
You are the last line of defense. No system is perfect. But your documented alert can be.
When to Revisit Your Safety Alerts
Don’t set it and forget it. Review your list:- Every time you see a new doctor or pharmacist
- After any hospital stay
- When you start or stop any medication-even vitamins or herbal supplements
- Every six months, even if nothing changed
Also, check the FDA’s MedWatch website monthly for updates on your drugs. If you see a new alert, update your list within 48 hours.

How This Helps Your Care Team
Your documented safety alerts aren’t just for you. They’re for the nurse giving your IV, the pharmacist filling your prescription, the paramedic responding to your fall. When every member of your care team sees the same clear warning, they can act fast.One study showed that when patients brought a documented safety alert list to the ER, staff were 70% more likely to catch a dangerous interaction before it caused harm. That’s not luck. That’s clarity.
What’s Next: Automated Alerts Are Coming
In 2025, hospitals and pharmacies are starting to use AI tools that automatically update safety alerts based on FDA notices and patient data. But these systems aren’t perfect yet. Early versions missed 18% of critical alerts. So until your pharmacy or app has a foolproof system, your handwritten or printed alert is still the most reliable tool you have.The goal isn’t to overwhelm yourself with notes. It’s to make sure the most dangerous risks are impossible to overlook. One red line. One clear phrase. That’s all it takes to prevent a tragedy.
What if I don’t know if my medication is high-risk?
Check the ISMP’s official list of high-alert medications at ismp.org. You can also ask your pharmacist directly: “Is this a high-alert drug?” If they hesitate, ask for the ISMP guidelines. Common ones include insulin, opioids, heparin, methotrexate, and IV potassium. If you’re on chemotherapy, it’s automatically high-risk.
Can I use my phone app to document safety alerts?
Some apps let you add custom notes, but most don’t make alerts stand out enough. If your app doesn’t let you use color, bold text, or sticky flags next to the drug name, it’s not reliable. Print a paper copy and keep it with you. Digital is helpful, but paper is fail-safe.
Should I include over-the-counter drugs and supplements?
Yes. Especially if you’re on blood thinners, diabetes meds, or kidney medications. Supplements like St. John’s Wort, ginkgo, or high-dose vitamin E can interact dangerously. Add a note: “Avoid ibuprofen, aspirin, or fish oil unless approved by doctor.”
What if my doctor says the alert isn’t necessary?
Ask them to show you the official warning from the drug manufacturer or ISMP. If they can’t, insist on documenting it anyway. You’re the one taking the risk. Your safety isn’t optional. If they refuse, get a second opinion from a pharmacist or another doctor.
How often should I update my medication list?
Update it every time you start, stop, or change the dose of any medication-even a vitamin. Also update it every six months, even if nothing changed. And always update it within 48 hours of seeing a new FDA safety alert for any of your drugs.