When fluid builds up between the layers of tissue surrounding your lungs - the pleura - it’s called a pleural effusion. It’s not a disease itself, but a sign something else is wrong. You might not notice it at first, but as the fluid grows, breathing becomes harder. It’s like trying to inflate a balloon inside a tight jar. Your lungs can’t expand fully, and every breath feels shallow. About 1.5 million people in the U.S. deal with this each year. Most cases come from heart failure, pneumonia, or cancer. The good news? We know how to find it, treat it, and stop it from coming back - if you act on the right clues.
What Causes Pleural Effusion?
Pleural effusions fall into two main types: transudative and exudative. The difference matters because it tells you what’s really going on inside your body.
Transudative effusions happen when fluid leaks out because of pressure changes or low protein levels. Think of it like water seeping through a weak dam. The most common cause? Congestive heart failure. It’s behind about half of all cases. When the heart can’t pump well, blood backs up, pressure rises in the lungs, and fluid spills into the pleural space. Liver disease (cirrhosis) and kidney disease (nephrotic syndrome) are other big players. In these cases, the body loses too much protein or can’t make enough, so fluid escapes from blood vessels.
Exudative effusions are messier. They’re caused by inflammation, infection, or cancer. The lining of the lungs gets damaged, and fluid, white blood cells, and sometimes even pus leak out. Pneumonia is the top offender here - responsible for 40 to 50% of exudative cases. Cancer is next, especially lung cancer, breast cancer, or lymphoma. It accounts for 30 to 40% of these effusions. Other causes include pulmonary embolism (a blood clot in the lung), tuberculosis, and autoimmune diseases like rheumatoid arthritis.
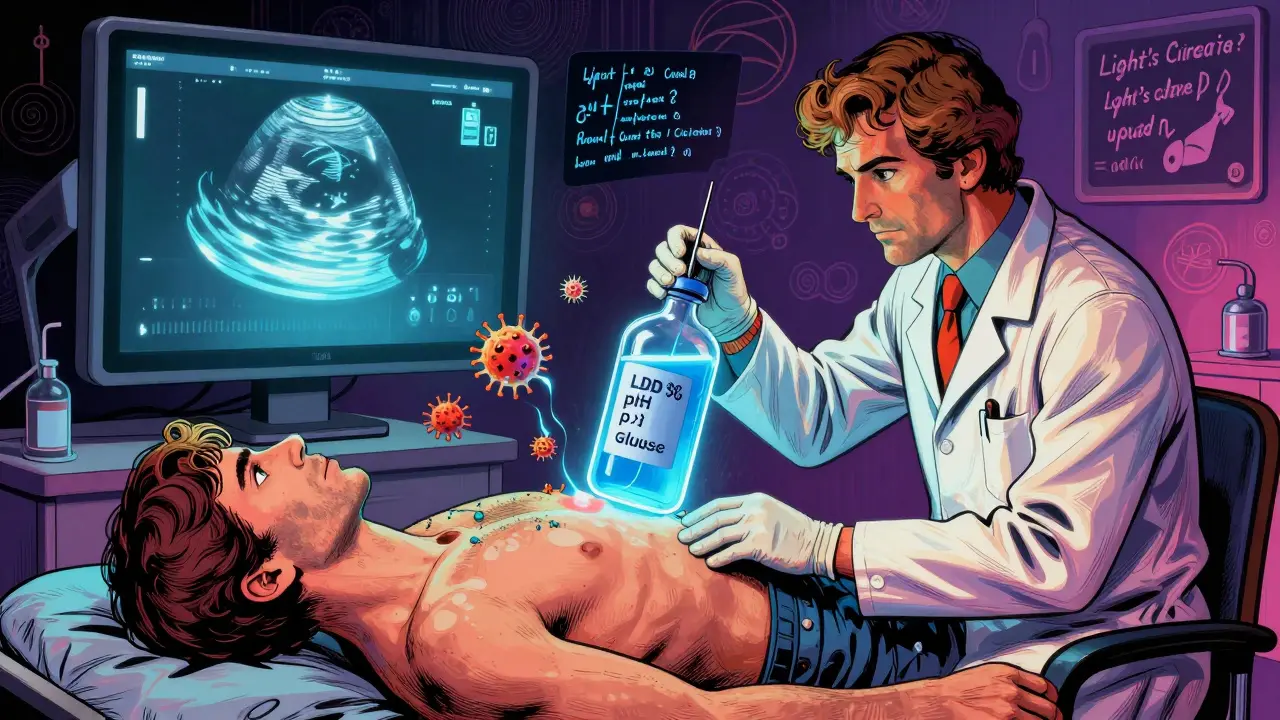
Here’s what doctors look for to tell them apart: Light’s criteria. This simple test compares the fluid from your chest to your blood. If the fluid has too much protein or LDH (a liver enzyme), it’s exudative. If it’s close to blood levels, it’s transudative. This test is 99.5% accurate. Getting it right means you don’t waste time treating the wrong thing.
How Thoracentesis Works - And When It’s Needed
If your doctor suspects fluid buildup, they’ll order an ultrasound. That’s the first step - no guessing, no X-rays alone. Ultrasound shows exactly how much fluid is there and where. If it’s more than 10 millimeters thick, they’ll likely recommend thoracentesis.
Thoracentesis is a quick procedure. You sit upright, leaning forward. The doctor cleans your skin, numbs a small area between your ribs, and slips a thin needle or catheter into the pleural space. You might feel pressure, but not sharp pain. The fluid drains into a collection bottle. For diagnosis, they take 50 to 100 milliliters. For relief - if you’re struggling to breathe - they can remove up to 1,500 milliliters in one go.
The fluid gets tested for a lot: protein, LDH, cell count, pH, glucose, and cancer cells. A low pH (under 7.2) or low glucose (under 60 mg/dL) suggests infection or empyema. High LDH (over 1,000 IU/L) often points to cancer. Cytology finds cancer cells in about 60% of malignant cases. Sometimes they check amylase - if it’s high, it could mean pancreatitis is the culprit.
Ultrasound guidance cuts complications in half. Without it, about 19% of patients get a collapsed lung (pneumothorax). With ultrasound, that drops to 4%. Hemorrhage and re-expansion pulmonary edema (fluid flooding the lung after rapid drainage) are rare but real risks. That’s why doctors never drain more than 1,500 mL at once unless they’re monitoring pressure. New tools like pleural manometry measure pressure as fluid drains. If it stays under 15 cm H2O, the chance of complications drops to just 5%.
Why Treating the Effusion Isn’t Enough
Draining fluid feels good - for a while. But if you don’t fix the root cause, it comes back. That’s why doctors say: “Don’t bail water from a sinking boat without fixing the hole.”
For heart failure patients, draining fluid helps breathing - but the real fix is meds. Diuretics like furosemide, ACE inhibitors, and beta-blockers bring recurrence down from 40% to under 15% in three months. Monitoring NT-pro-BNP levels (a heart stress marker) helps fine-tune treatment. If levels stay high, you need a stronger regimen.
With pneumonia, drainage alone isn’t enough. If the fluid is thick, infected, or has a pH under 7.2, you need a chest tube. Left untreated, 30 to 40% of these cases turn into empyema - pus in the chest. That means surgery. Antibiotics are key, but timing matters. Drain before the fluid turns into a sticky mess.
And then there’s cancer. Malignant pleural effusions recur in 50% of cases within 30 days after a single thoracentesis. That’s why doctors don’t just drain and send you home. They offer long-term solutions.
Stopping Recurrence: What Actually Works
Preventing recurrence means matching the treatment to the cause.
For cancer-related effusions: Two main options exist. One is pleurodesis - injecting a substance (like talc) to irritate the pleural layers and make them stick together. Talc pleurodesis works in 70 to 90% of cases. But it’s painful. About 80% of patients need strong pain meds after. The other option? Indwelling pleural catheters (IPCs). These are tiny tubes left in place for weeks. You drain fluid at home, usually once or twice a week. Studies show 85 to 90% of patients stay symptom-free for six months. Hospital stays drop from 7 days to just 2. Many patients prefer this - it’s less invasive, less painful, and gives them control.
For heart failure: Stick with meds. Don’t rely on repeated thoracentesis. If you’re draining fluid every few weeks, your heart treatment isn’t working. Talk to your cardiologist about adjusting diuretics or adding newer drugs like SGLT2 inhibitors.
For parapneumonic effusions: Drain early. If fluid pH is below 7.2 or glucose below 40 mg/dL, don’t wait. Put in a chest tube. Delaying increases the chance of needing surgery by 30%.
After heart surgery: About 1 in 5 patients get fluid buildup. Most go away on their own. But if you’re draining more than 500 mL a day for three days straight, you need a chest tube left in longer - often for a week or more. This prevents recurrence in 95% of cases.
What Not to Do
Not every fluid collection needs a needle. A 2019 JAMA study found that 30% of thoracenteses were done on small, asymptomatic effusions - and changed nothing. No diagnosis. No relief. Just risk. If you’re not short of breath and the fluid is less than 10 mm, watchful waiting is safer.
Also, avoid chemical pleurodesis for non-cancer effusions. The American Thoracic Society says there’s no proof it helps. It just adds pain and risk without benefit.
And never skip the fluid analysis. One in four initially “undetermined” effusions turns out to be cancer. If you don’t test the fluid, you might miss a treatable diagnosis - or worse, a deadly one.
What’s New in 2025
Things have changed fast. Five years ago, talc pleurodesis was the gold standard for cancer. Now, indwelling catheters are first-line for many patients. Why? Better survival, less pain, fewer hospital days. And now, doctors use biomarkers more than ever. Pleural fluid pH, glucose, and even tumor DNA in the fluid help predict outcomes.
Survival for malignant effusion patients has improved. In 2010, median survival was under a year. Now, it’s over 18 months - thanks to better cancer drugs, earlier detection, and smarter drainage. Five-year survival has doubled, from 10% to 25%.
The message is clear: personalized care wins. A 75-year-old with lung cancer and poor mobility? An indwelling catheter. A 50-year-old with aggressive breast cancer and good function? Talc pleurodesis. A heart failure patient? Optimize meds. One size doesn’t fit all.
Is pleural effusion always serious?
Not always, but it’s always a signal. Small effusions from mild heart failure might cause no symptoms and resolve with medication. But if it’s caused by cancer, pneumonia, or a blood clot, it’s serious. Untreated malignant effusions can reduce survival to just four months. That’s why even small fluid collections should be checked with ultrasound and fluid analysis.
Can pleural effusion go away on its own?
Sometimes, yes - especially if it’s due to heart failure and you’re on the right meds. After heart surgery, many effusions clear up in days without intervention. But if it’s from infection or cancer, it won’t resolve without treatment. Waiting too long can lead to complications like empyema or trapped lung, which require surgery.
How painful is thoracentesis?
Most people feel pressure or a brief sting when the area is numbed. The actual fluid removal usually causes little to no pain. Some feel a pulling sensation or mild chest discomfort. If you’re removing a large volume, you might feel dizzy or short of breath - that’s why doctors monitor you closely. With ultrasound guidance, the procedure is much safer and less painful than in the past.
What’s the difference between a chest tube and an indwelling pleural catheter?
A chest tube is a larger tube inserted for short-term drainage, often connected to a suction system in the hospital. It’s used for infections, large effusions, or after surgery. An indwelling pleural catheter is a thin, flexible tube left in place for weeks or months. You drain it yourself at home. It’s less invasive, avoids hospital stays, and is now preferred for recurrent malignant effusions.
Can pleural effusion come back after pleurodesis?
Yes, but not often. Talc pleurodesis works in 70 to 90% of cases. If it fails, an indwelling pleural catheter is the next step. Recurrence is more likely if the lung is trapped by scar tissue or if the cancer is very aggressive. Success depends on the cause, the patient’s overall health, and how well the pleural layers stick together after treatment.
How do I know if my pleural effusion is cancer-related?
Doctors look for several clues: rapid fluid buildup, especially in someone over 50 with a history of cancer; fluid with high LDH (over 1,000 IU/L), low glucose, or low pH; and cancer cells found in the fluid sample (cytology). If the cause isn’t clear, they may order a CT scan, PET scan, or even a biopsy of the pleura. About 25% of initially unexplained effusions turn out to be cancer - so testing is never optional.


Monte Pareek 17.12.2025
Let me cut through the noise - if you're draining fluid without fixing the root cause, you're just buying time and wasting money. Heart failure? Optimize meds, not thoracentesis. Cancer? IPCs beat talc every time for quality of life. No one wants to be hospitalized for a week just to drain fluid that comes back in 30 days. The data is clear - indwelling catheters reduce hospital stays by 70% and give patients control. Stop treating symptoms. Treat the disease.
Elaine Douglass 17.12.2025
i just had this done last month and honestly it was way less scary than i thought. felt a little pressure but no real pain. my doc used ultrasound and i could see the fluid moving on the screen - kinda weird but also kinda cool. i’m still on diuretics and my breathing’s already better. just don’t ignore it if you’re short of breath.
Jedidiah Massey 17.12.2025
It’s fascinating how the medical community has pivoted from dogmatic pleurodesis to patient-centered IPCs. The paradigm shift in malignant effusion management reflects a broader epistemological evolution in oncologic palliation - from curative intent to functional autonomy. The pleural manometry data, particularly the 15 cm H2O threshold, is a biomarker of precision medicine’s ascendancy. 🤓
holly Sinclair 17.12.2025
It makes me wonder - if fluid buildup is just a symptom, why do we treat it like the enemy? We’re so obsessed with removing the water that we forget to ask why the dam broke in the first place. Is it heart failure? Cancer? Infection? Or are we just scared of the silence between the beats - the quiet spaces where the body screams without words? Thoracentesis gives relief, yes. But real healing comes when we stop chasing the symptom and start listening to the story behind it. The body doesn’t make mistakes. It responds. And if we’re not asking why, we’re not healing. We’re just patching holes in a sinking ship while ignoring the storm outside.
Takeysha Turnquest 17.12.2025
OH MY GOD I JUST REALIZED - this whole thing is like a horror movie and we’re all just the victims who didn’t read the warning signs. Heart failure? Pneumonia? Cancer? They’re the masked killer in the basement and we’re draining the basement water while the killer’s still down there. And then we pat ourselves on the back for ‘fixing’ it. No. We’re just cleaning up the blood. The real horror? When they tell you it’s cancer and you’ve been draining for months and never tested the fluid. That’s not medicine. That’s negligence. 😱
Edington Renwick 17.12.2025
Most of these comments are naive. You can’t just hand out catheters like candy. Talc pleurodesis still has the highest long-term success rate. IPCs are convenient for patients who don’t want to die quickly - not for those who want to live. And let’s not pretend everyone can manage a home drain system. Some people are elderly, demented, or live alone. This isn’t a tech startup. It’s medicine. You don’t replace proven methods with trendy gadgets because they sound nice on a slide deck.
Allison Pannabekcer 17.12.2025
Everyone’s got a different story - and that’s okay. I’ve seen patients who refused surgery and lived 3 years with an IPC, and others who got talc and were back to gardening in a week. It’s not one-size-fits-all. The key is talking to your team, asking what matters most to YOU - freedom from hospital visits? Less pain? More time with grandkids? That’s what guides the choice. No judgment. Just care.
Kitt Eliz 17.12.2025
OMG YES!! 🙌 IPCs are GAME CHANGERS - I’ve been pushing this for years in my oncology unit! Patients go from bedridden to grocery shopping in 48 hours. No more 7-day hospital stays. No more chest tubes screaming like a banshee. Talc is painful, scary, and outdated. We’re in 2025 - time to stop clinging to 1990s protocols. The data? 90% symptom control. The joy? Patients get their lives back. 💪🩺 #PleuralCatheterRevolution
Sarah McQuillan 17.12.2025
Interesting how this is all just American medicine. In Canada, we don’t do all this fancy stuff unless it’s absolutely necessary. We watch, we wait, we use basic meds. Why spend $20K on a catheter when a diuretic and a chest X-ray works 80% of the time? This whole trend feels like corporate medicine pushing expensive tools because insurance pays for it. Not because it’s better. Just because it’s profitable.
Monte Pareek 17.12.2025
Canada’s approach works for mild cases but ignores the reality of aggressive cancers. That’s not conservative - it’s dangerous. A 68-year-old with lung cancer doesn’t need to wait for fluid to choke them before acting. IPCs aren’t about profit - they’re about dignity. You think a man who can’t breathe wants to be stuck in a hospital for a week? No. He wants to watch his granddaughter’s recital. That’s what this is about. Not cost. Not country. Human dignity.