Genetic Drug Response: How Your DNA Affects Medication Effectiveness
When a drug doesn’t work for you—or makes you sick—blaming bad luck isn’t enough. Your genetic drug response, how your body reacts to medications based on inherited DNA differences. Also known as pharmacogenomics, it explains why two people taking the same pill can have totally different outcomes. This isn’t science fiction. It’s happening right now in clinics and kitchens across the country, where someone’s antidepressant fails while their neighbor feels fine, or a painkiller gives one person relief and another vomiting.
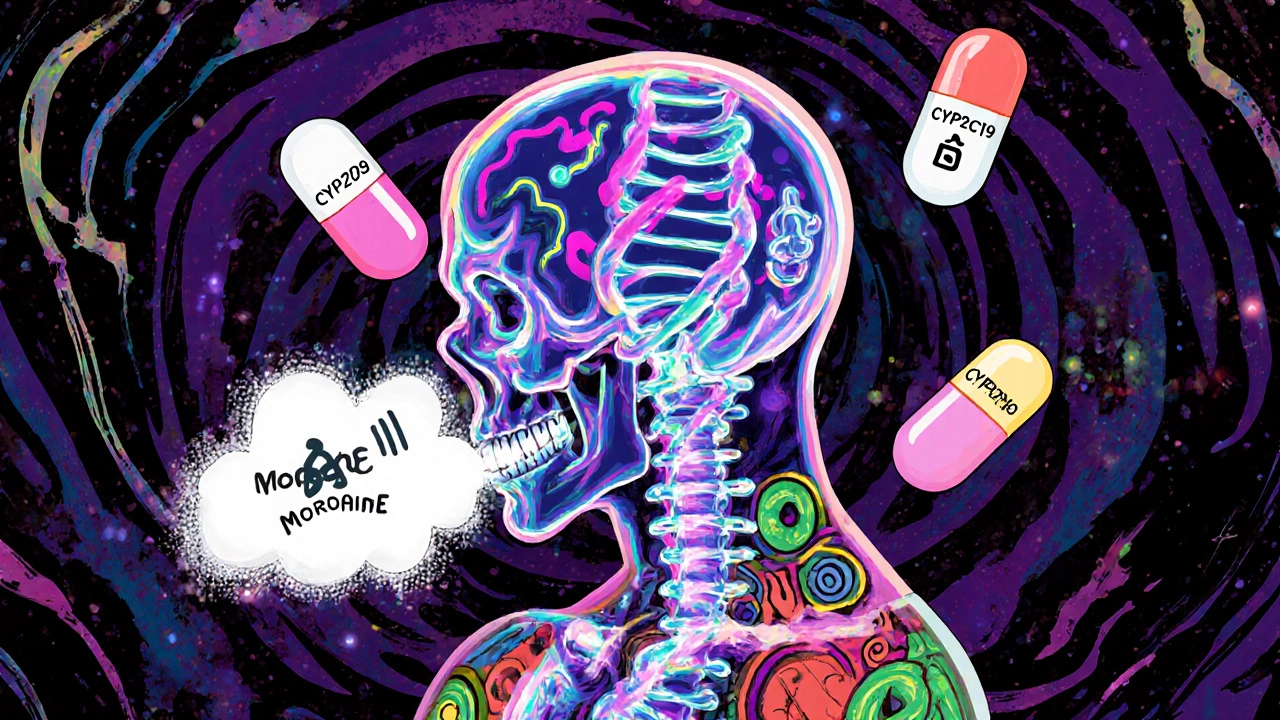
The real issue? Most doctors still prescribe based on weight, age, or symptoms—not your genes. But your body’s ability to break down drugs, absorb them, or even target them to the right cells is coded in your DNA. Certain gene variants like CYP2D6, CYP2C19, and SLCO1B1 control how fast or slow you metabolize common drugs—from blood thinners to statins to SSRIs. Slow metabolizers? They get too much drug built up, risking side effects. Fast metabolizers? The drug vanishes before it can help. That’s why you might need twice the dose of a medication your cousin swears by.
This isn’t just about effectiveness—it’s about safety. A single wrong dose of warfarin can cause internal bleeding. A standard dose of codeine might be deadly for a child with a super-active CYP2D6 gene. Even something as simple as taking statins can lead to muscle damage if you carry a specific SLCO1B1 variant. And it’s not rare. Studies show over 90% of people carry at least one gene variant that affects how they respond to one or more common medications. Yet, we keep giving the same scripts like they’re one-size-fits-all shoes.
What you’ll find in these articles isn’t theory. It’s real-world connections: how genetic drug response ties into thyroid meds, psychiatric switches, kidney treatments, and even over-the-counter painkillers. You’ll see why changing antidepressants can feel like a mental rollercoaster—not because the drug is weak, but because your body handles it differently. You’ll learn why iron supplements mess with thyroid meds not just because of timing, but because of how your genes process both. And you’ll see how contamination in generics isn’t just a manufacturing flaw—it’s a genetic risk multiplier when your body is already sensitive.
There’s no magic pill that fixes everything. But understanding your genetic drug response gives you power. It turns guesswork into strategy. It helps you ask the right questions, push for testing, and avoid years of trial-and-error that could’ve been avoided. The posts below don’t just list facts—they connect the dots between your genes, your meds, and your daily life. What works for someone else? It might not work for you. And now you know why.