Personalized Medicine: Tailored Treatments for Your Body and Condition
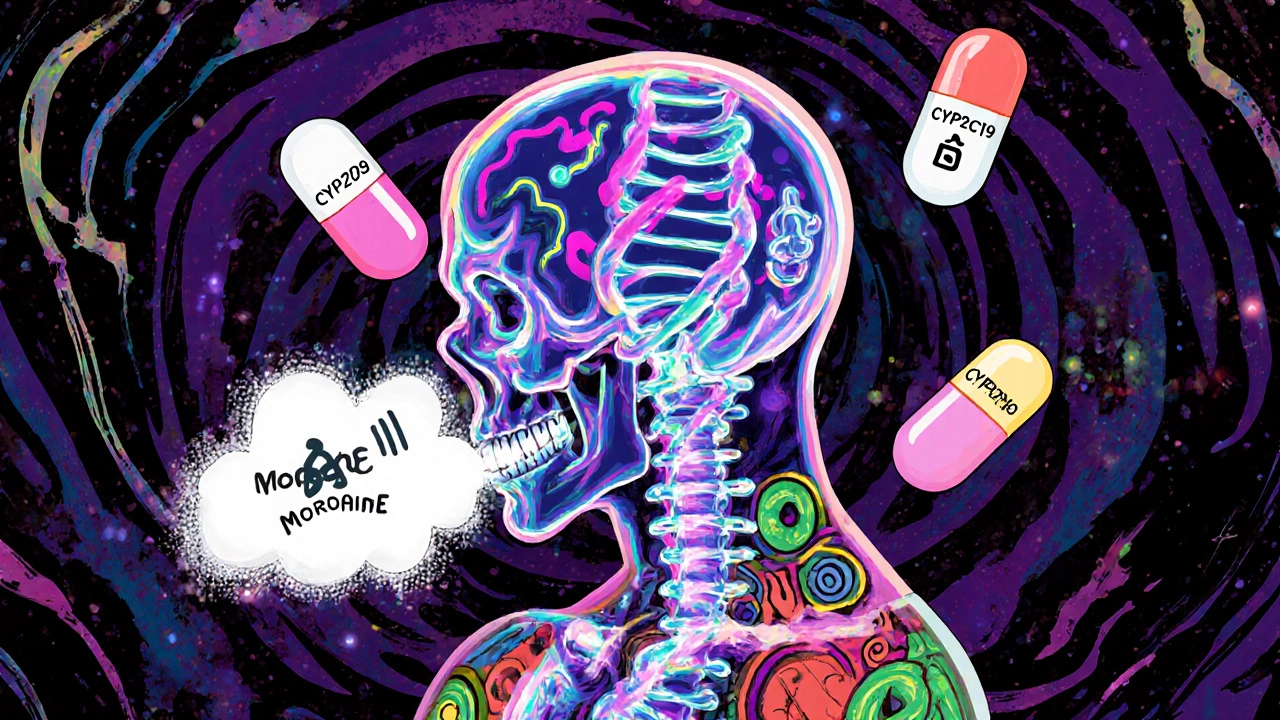
When you hear personalized medicine, a healthcare approach that customizes treatment based on your genes, lifestyle, and health history. Also known as precision medicine, it moves away from the old idea that one pill works for everyone. Instead, it asks: What works for you?
This isn’t science fiction—it’s happening right now. For example, someone with thyroid issues might need to time iron-rich meals carefully to avoid blocking levothyroxine, while another person with kidney disease gets IV iron and erythropoietin because their body doesn’t make enough of it. These aren’t random fixes—they’re responses to what your body actually needs. That’s personalized medicine in action: matching the right drug, dose, and timing to your unique biology.
It’s not just about genes. Your age, liver function, even your gut bacteria can change how a drug behaves in your system. That’s why switching psychiatric meds can trigger emotional side effects—even if the new drug is labeled "equivalent." Or why children’s dosing isn’t just a smaller adult dose—it’s calculated by weight, not age. And when you’re dealing with conditions like autonomic neuropathy or lupus flares triggered by infections, your treatment plan has to adapt to your body’s signals, not the other way around.
What makes personalized medicine different?
Traditional medicine often treats symptoms the same way across patients. Personalized medicine looks deeper: Why does this drug work for your cousin but make you dizzy? Why does your kidney disease need a different iron protocol than someone else’s? It uses tools like genetic testing to predict how you’ll respond to a drug, or tracks your real-time symptoms to adjust treatment. That’s why newer antidepressants like Zuranolone or SPRAVATO are being studied not just for effectiveness, but for who they help most—and who might get worse.
It’s also why fixed-dose combinations exist: putting two meds in one pill isn’t just convenient—it’s designed to match your specific condition profile. And when contamination controls in generic drug manufacturing matter, it’s because a tiny impurity could trigger a reaction in someone with a rare genetic sensitivity.
What you’ll find below isn’t a list of random drug guides. It’s a collection of real-world examples showing how personalized medicine works in practice: from how oxymetazoline affects your focus (it doesn’t—it just helps you breathe better), to why someone with presbycusis needs different hearing aids than their neighbor, to how canagliflozin might lift or drag your mood. These aren’t general advice pieces. They’re snapshots of care tailored to individual biology, lifestyle, and response. You’re not just reading about drugs—you’re seeing how medicine is finally catching up to the fact that no two bodies are the same.