Scabies Treatment: What Works, What Doesn’t, and How to Avoid Reinfestation
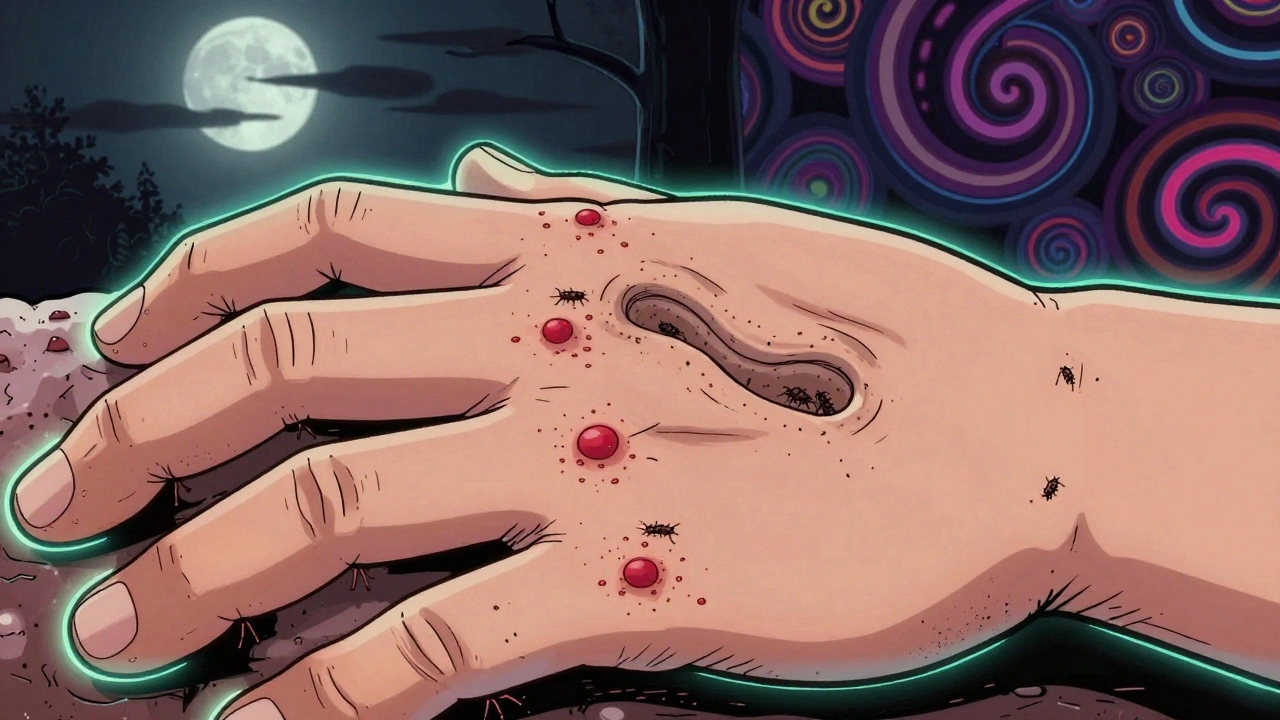
When you have scabies, a skin infestation caused by the Sarcoptes scabiei mite. Also known as the seven-year itch, it’s not about poor hygiene—it’s about close contact. These tiny mites burrow into your skin, lay eggs, and trigger intense itching, especially at night. Without proper scabies treatment, a targeted medical approach to kill mites and their eggs, the cycle keeps going—and so does the spread.
Most doctors start with permethrin cream, a topical pesticide approved by the FDA for scabies. It’s applied from the neck down, left on overnight, and washed off the next morning. It kills mites and eggs, but it won’t stop itching right away—that’s your body’s reaction, not live mites. If permethrin doesn’t work or you can’t use it (like if you’re pregnant or have sensitive skin), ivermectin, an oral antiparasitic drug is often prescribed. It’s not FDA-approved for scabies in the U.S., but doctors use it off-label all the time, especially for crusted scabies or outbreaks in group settings.
Here’s what most people get wrong: treating only yourself. Scabies spreads through skin-to-skin contact, so everyone who’s had close contact—roommates, partners, kids, even grandparents who held your baby—needs treatment at the same time. Even if they’re not itchy yet. Mites can live on bedding, towels, and clothes for up to 72 hours. That’s why washing everything in hot water and drying on high heat isn’t optional—it’s essential. Items you can’t wash? Seal them in plastic bags for a week. No shortcuts.
Over-the-counter lotions, tea tree oil, or sulfur ointments from the pharmacy? Some help with itching, but none reliably kill mites like permethrin or ivermectin. Don’t waste time on home remedies if you’ve been diagnosed. And don’t assume the itching means the treatment failed. It can last weeks after the mites are gone. If itching doesn’t improve after two weeks, or new burrows appear, you might need a second round of treatment—or a different one.
Scabies outbreaks in nursing homes, schools, or shelters aren’t rare. They happen fast. That’s why knowing the signs—thin, wavy lines on skin, clusters of bumps, itching worse at night—is key. Early treatment stops bigger outbreaks. It’s not embarrassing. It’s medical. And it’s fixable.
Below, you’ll find real posts from people who’ve been through it—what worked, what didn’t, and how they finally got relief. No fluff. Just facts from real cases and medical guidance you can trust.