Imagine breaking out in tiny, burning bumps the moment you start jogging, walking into a warm room, or even eating a spicy meal. No allergens. No poison ivy. Just your own body overheating-and your skin reacting like it’s under attack. That’s cholinergic urticaria, or heat hives, a real and often misunderstood condition affecting up to 7% of people who get hives. It’s not an allergy to heat. It’s your nervous system misfiring when your core temperature rises, triggering a flood of histamine that turns your skin into a map of angry red dots.
What Exactly Are Heat Hives?
Cholinergic urticaria isn’t just a rash. It’s a specific type of physical urticaria-meaning it’s triggered by a physical stimulus, not a food, pollen, or pet dander. The trigger? Any rise in body temperature that makes you sweat. That could be exercise, hot showers, spicy food, stress, or even a crowded room. The reaction is fast: within 2 to 15 minutes, you’ll see 1-3 millimeter red bumps, often surrounded by a red flare. They itch, tingle, and feel warm to the touch. Unlike regular hives, these don’t last long-usually 15 to 30 minutes-and fade completely within 90 minutes once you cool down.
The worst part? These hives show up where you sweat most: chest (78% of cases), face (65%), upper back (62%), and arms (58%). You won’t usually see them on your palms or soles. And while they look harmless, they can be more than an annoyance. About 12% of people with cholinergic urticaria experience systemic symptoms-dizziness, rapid heartbeat, low blood pressure, or even trouble breathing. For 9% of patients, this escalates to a risk of anaphylaxis, requiring an epinephrine auto-injector.
Why Does This Happen?
It’s not your immune system attacking something foreign. It’s your nerves and sweat glands sending mixed signals. When your body heats up, nerve fibers around your sweat glands release acetylcholine, a chemical that normally tells your glands to produce sweat. In people with cholinergic urticaria, something goes wrong. Their skin cells don’t break down acetylcholine efficiently, and their mast cells (the immune cells that release histamine) overreact to the signal. Research shows low levels of an enzyme called acetylcholinesterase and high levels of inflammatory chemokines in sweat gland tissue are to blame.
This is why antihistamines work-they block histamine, the main culprit behind the itching and swelling. But it’s not an allergy. You can’t avoid it by staying away from a trigger like peanuts or cats. The trigger is your own body temperature. And that’s unavoidable. You need to sweat to cool down. You need to move to stay healthy. You need to eat to live. That’s what makes this condition so hard to manage.
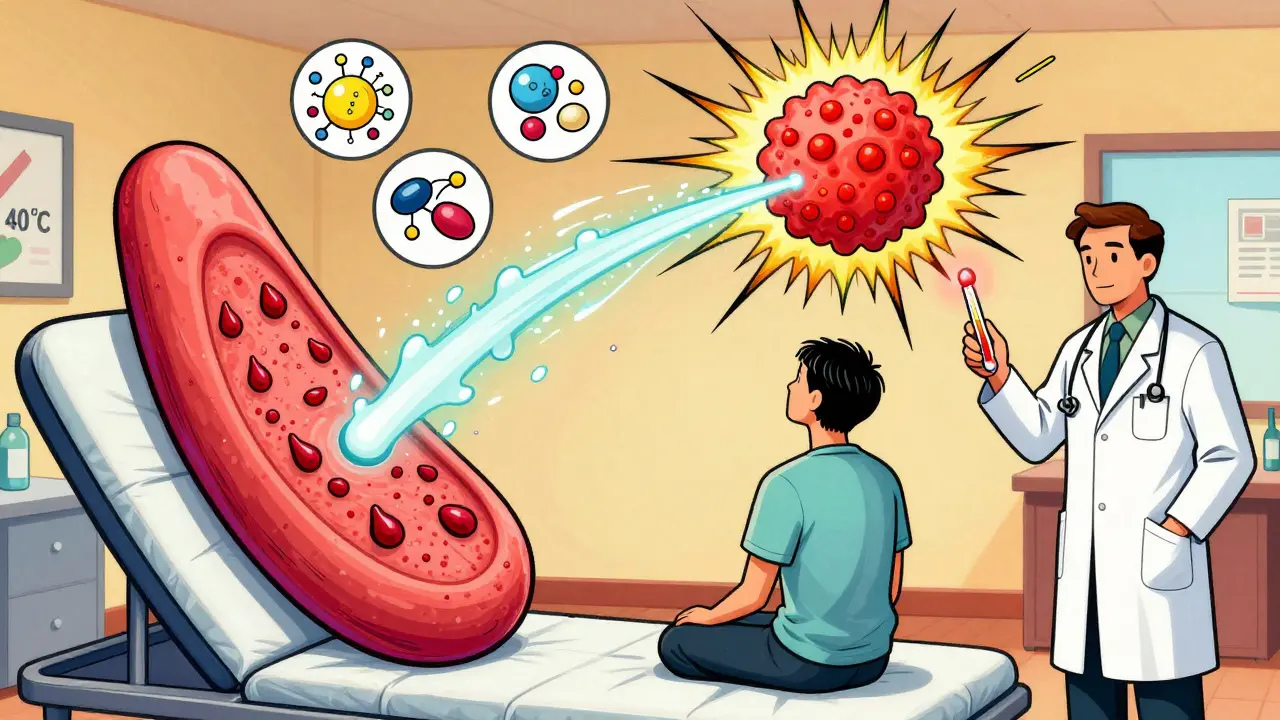
How Is It Diagnosed?
Doctors don’t rely on blood tests or skin prick tests for cholinergic urticaria. The gold standard is the passive warming test. You sit in a warm room (usually around 40°C or 104°F) while your core temperature is slowly raised by 0.5°C. If you develop the classic pinpoint hives within minutes, the diagnosis is confirmed. This test works in 94% of cases.
Many people are misdiagnosed. Emergency rooms often mistake cholinergic urticaria for exercise-induced anaphylaxis. The difference? In anaphylaxis, symptoms come from a food or medication trigger combined with exercise. In cholinergic urticaria, it’s just the heat and sweat. Getting the right diagnosis matters because treatment is completely different.
What Triggers It? (And What Doesn’t)
Not all heat is equal. You don’t need to be in a sauna to trigger it. For most people, the trigger kicks in when core body temperature hits around 38.1°C (100.6°F)-just slightly above normal. Here’s what commonly sets it off:
- Exercise (83% of cases-running, cycling, even brisk walking)
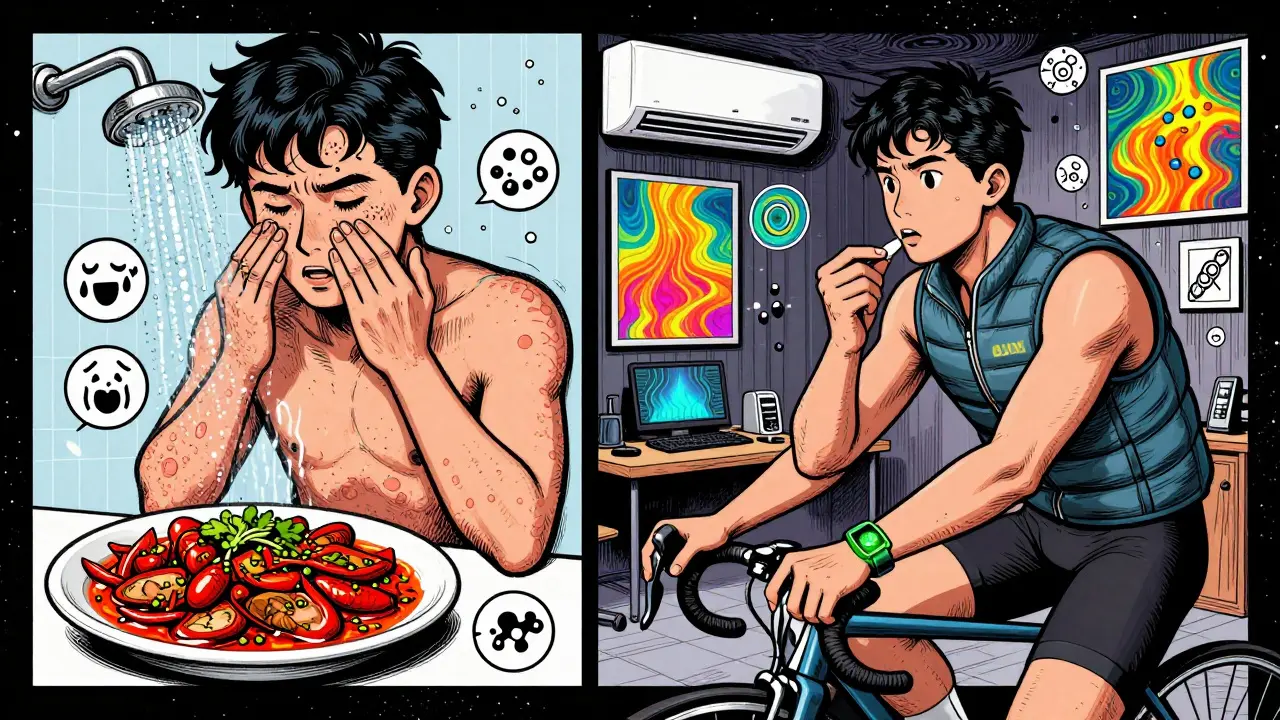
- Hot showers or baths
- Spicy foods (67% of patients report this as a secondary trigger)
- Emotional stress or anxiety
- Wearing tight or non-breathable clothing
- Hot weather or humid environments
What doesn’t trigger it? Cold temperatures. Sunlight. Pressure from clothing. These cause other types of urticaria, but not cholinergic. If your hives show up only after a sunburn or from tight jeans, you likely have a different condition.
How to Prevent and Manage Heat Hives
You can’t stop your body from heating up-but you can control how fast it heats and how well it cools. Prevention is about managing your thermal load.
1. Control Your Environment
Work out in air-conditioned spaces. Use fans. Avoid exercising during peak heat hours. If you’re outside, choose shaded paths and wear lightweight, moisture-wicking fabrics. Cotton traps sweat. Synthetic blends like polyester or nylon pull it away from your skin and dry faster. Some people swear by cooling vests or wearable tech like ThermaCare’s prototype garments, which reduce flare frequency by over 60% in early testing.
2. Pace Your Activity
Don’t go from zero to sprint. Start slow. Let your body adjust. Many people find that warming up gently for 10 minutes before intense activity reduces or eliminates outbreaks. If you feel the first tingle, stop. Cool down immediately. Splash cold water on your neck. Step into a shaded area. Don’t push through it.
3. Watch Your Diet
Spicy foods are a major trigger for two-thirds of people. Capsaicin in chili peppers raises your internal temperature. If you notice hives after curry, hot wings, or even wasabi, cut back. Alcohol and hot beverages can also contribute. Stay hydrated with cool water-not sugary drinks or caffeine, which can dehydrate you and raise your core temperature.
4. Use the Right Medication
Second-generation antihistamines are the first-line treatment. Cetirizine (Zyrtec) or loratadine (Claritin) taken daily can reduce flare frequency by 68%. If standard doses don’t work, doctors may increase the dose up to four times the normal amount (e.g., 40mg of cetirizine daily). That’s safe for most people and often effective.
If antihistamines alone aren’t enough, adding an H2 blocker like famotidine (Pepcid) 20mg twice daily helps 57% of resistant cases. For severe, persistent cases, omalizumab (Xolair)-a biologic used for asthma and chronic hives-was approved for cholinergic urticaria in Europe in 2023. It’s expensive ($3,500/month in the U.S.), but for some, it’s life-changing.
What Doesn’t Work
Don’t waste time on unproven remedies. Cold compresses help once the hives start, but they won’t prevent them. Antihistamine creams? Useless-they don’t penetrate deep enough. Avoiding all exercise? Not sustainable. You’ll lose fitness, gain weight, and your body will become even more sensitive to heat.
First-generation antihistamines like diphenhydramine (Benadryl) cause drowsiness and aren’t recommended for daily use. Over 58% of patients report they can’t function at work or school while taking them.
Living With It: Real-Life Impact
People with cholinergic urticaria don’t just deal with itchy skin. They deal with isolation. One Reddit user missed 14 weddings in three years because formal attire traps heat. Another couldn’t attend her daughter’s school play because the auditorium was too warm. The emotional toll is real. Studies show 62% of patients report moderate to severe impact on quality of life-higher than most chronic skin conditions, except psoriasis.
But many find control. One user switched to indoor cycling in a cooled studio and went from daily flares to 1-2 per month. Another started using a temperature-tracking app that logs body heat, activity, and symptoms. After 8 weeks, they identified their personal trigger point: 38.2°C. Now they know when to stop before it starts.
What’s Next?
Research is moving fast. Scientists are working on biomarkers to diagnose cholinergic urticaria with a simple blood test by 2026. Smart clothing that monitors core temperature in real time is in development and could alert you before you overheat. Climate change may make this condition more common-rising global temperatures could increase prevalence by 15-25% in temperate zones by 2040.
For now, the best strategy is simple: know your triggers, cool down before you overheat, and take your meds consistently. You don’t have to give up life. You just need to manage it smarter.


Vince Nairn 6.01.2026
so i got these little red dots after a jog and thought i was allergic to sweat lmao turns out my body just hates being alive
turns out i'm not broken just overworked and under-ventilated
Adam Gainski 6.01.2026
This is actually one of the better explainers I've seen on cholinergic urticaria. The passive warming test detail is gold-most docs skip that. Also, the H2 blocker combo tip? Lifesaver for people who can't tolerate high-dose antihistamines. I've seen patients go from daily flares to nearly zero with cetirizine + famotidine. No magic, just science.
Anastasia Novak 6.01.2026
oh wow someone actually wrote a 1000-word essay on why sweating makes you look like a human raspberry
congrats, you've turned a minor inconvenience into a medical documentary
next up: the tragic tale of my toe getting cold and my body betraying me with a single pimple
so dramatic
Elen Pihlap 6.01.2026
i feel you so much i cry every time i get these hives its not just the itch its the shame like why does my body do this to me i cant even go to the gym without looking like i got beat up by a bee swarm
Sai Ganesh 6.01.2026
In India, many dismiss this as 'heat allergy' and suggest ayurvedic cooling herbs. But the science here is solid. Acetylcholine buildup, not karma. I've seen patients in Delhi heatwaves with this-no one understands. The passive warming test is rarely done here. We need more awareness.
Katrina Morris 6.01.2026
i never knew this had a name i thought i was just weird until i saw someone else describe it exactly
spicy food triggers me too and i always thought it was just me being dramatic
cooling vests sound like a dream i need one like yesterday
steve rumsford 6.01.2026
so my body turns me into a walking rash every time i do laundry or eat tacos
apparently i'm not broken just overzealous with my sweat glands
also i tried benadryl once and slept for 14 hours so i just suffer in silence
Andrew N 6.01.2026
You missed the most important part. The real issue isn't the hives-it's that people don't realize this is neurological, not immunological. That's why antihistamines only help partially. The real fix is modulating acetylcholine breakdown, not blocking histamine. You're treating the symptom, not the signal.
LALITA KUDIYA 6.01.2026
i tried everything from cold showers to yoga in AC rooms
then i started taking 20mg cetirizine daily
no more flares
life is quiet now
thank you for writing this
Poppy Newman 6.01.2026
This is so important 🥹 I had no idea this was a real condition with a name. I thought I was just 'sensitive to heat' and that I needed to 'toughen up'. The part about anaphylaxis risk? Scary but necessary to know. I’m sharing this with my whole family now. 🙏