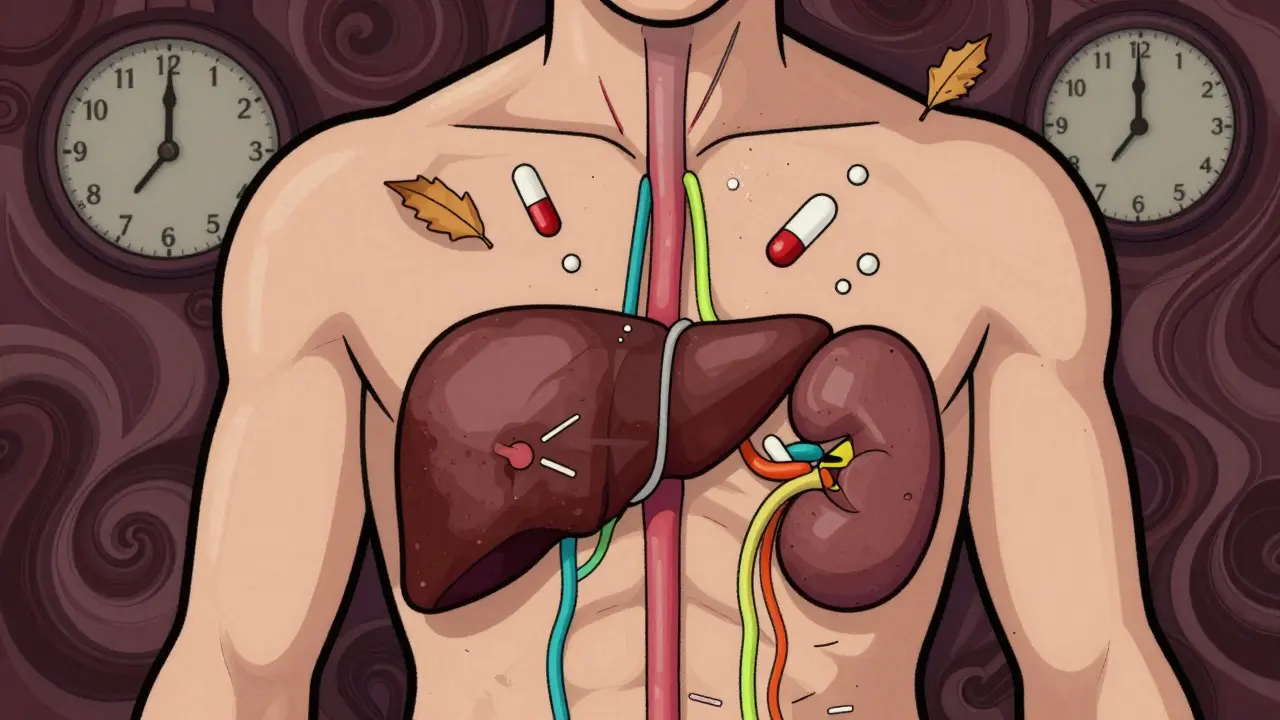
When you’re 70 or older, your body doesn’t process medications the same way it did at 30. That’s not just a myth-it’s biology. The liver and kidneys, two of your body’s main drug-processing organs, change with age. And those changes can turn a safe dose into a dangerous one. Many older adults end up in the hospital not because they took too many pills, but because the pills they took stayed in their system too long. The liver and kidney changes affecting drug metabolism in older adults are one of the most overlooked reasons for adverse drug reactions in seniors.
What Happens to the Liver as We Age?
Your liver shrinks. By the time you reach your 70s, it’s about 30% smaller than it was in your 20s. Blood flow to the liver drops by nearly 40%. These aren’t minor tweaks-they’re major shifts in how drugs are broken down. The liver uses enzymes, especially the cytochrome P450 family, to metabolize medications. Some of these enzymes slow down. Others don’t. It’s not a simple decline-it’s a messy, uneven one.Drugs like propranolol, lidocaine, and morphine are heavily dependent on liver blood flow. When that flow drops, clearance drops too. That means these drugs stick around longer. A standard dose meant for a 40-year-old can build up in an 80-year-old, causing dizziness, low blood pressure, or even heart rhythm problems. On the flip side, drugs like diazepam or phenytoin rely more on enzyme activity than blood flow. Their metabolism changes less, so they’re often safer-unless you’re taking multiple drugs that interact.
There’s another hidden problem: first-pass metabolism. Some drugs are designed to be broken down by the liver before they enter the bloodstream. When liver function declines, more of the drug gets through unchanged. That’s why drugs like verapamil or propranolol can become 25-50% more potent in older adults. A pill that once helped with blood pressure might now cause your heart to slow too much.
Kidney Changes: The Silent Culprit
Kidneys don’t just filter urine-they filter drugs out of your blood. Between ages 30 and 80, your glomerular filtration rate (GFR) drops by 30-50%. That’s not just a number on a lab report. It means drugs like digoxin, metformin, and many antibiotics stay in your system longer. Your kidneys aren’t working slower-they’re working less.Here’s the trap: doctors often check serum creatinine to estimate kidney function. But as you age, you lose muscle mass. Less muscle means less creatinine, even if your kidneys are failing. So a “normal” creatinine level can be dangerously misleading. That’s why the Cockcroft-Gault equation and the newer CKD-EPI formula are better tools-they account for age, weight, and sex. But not every doctor uses them.
And here’s something few people know: when kidneys slow down, the liver slows down too. Recent studies show that kidney impairment reduces the activity of liver enzymes like CYP3A4. So even if a drug is mainly cleared by the liver, poor kidney function can still cause it to build up. It’s a chain reaction-one organ failing pulls the other down with it.
Why Some Drugs Are Riskier Than Others
Not all medications are created equal when it comes to aging. Some are high-risk. Others are safer. The difference comes down to how they’re processed.- High-risk drugs: Warfarin, digoxin, benzodiazepines (like lorazepam), and opioids (like codeine). These have narrow therapeutic windows. A little too much = serious side effects. In older adults, even small changes in metabolism can push them into toxicity.
- Lower-risk drugs: Many beta-blockers, ACE inhibitors like lisinopril (not perindopril-more on that later), and statins. These tend to be better tolerated, though they still need monitoring.
- Special case: Prodrugs: Drugs like perindopril or codeine need to be converted by the liver into their active form. If liver function is down, the conversion slows. You might not get the benefit you expect. Or worse-you take more because you don’t feel it working, and then suddenly, too much active drug floods your system.
Over-the-counter meds are just as dangerous. Acetaminophen (Tylenol) is the #1 cause of acute liver failure in older adults. Why? Because the liver’s ability to detoxify it drops with age. Even 3,000 mg a day-what some consider “safe”-can be too much. The FDA recommends no more than 2,600 mg daily for seniors, but most people don’t know that.

Real Stories Behind the Numbers
A 78-year-old woman started taking amitriptyline for nerve pain. Standard dose: 25 mg at night. Within a week, she was falling, confused, and barely able to stand. Her doctor assumed it was dementia. It wasn’t. Her liver couldn’t clear the drug. Her blood levels were triple the normal range. Once the dose was cut to 10 mg, she improved in days. A 72-year-old man with diabetes was prescribed metformin. His creatinine looked normal. But his GFR was only 40 mL/min. He developed lactic acidosis-a rare but deadly side effect. He survived, but barely. His case was caught because his pharmacist caught the mismatch between his age, kidney function, and the dose. These aren’t rare. They’re common. The FDA says 10% of hospital admissions in people over 65 are due to bad drug reactions. And 88% of those cases involve people taking five or more medications. Polypharmacy isn’t just about quantity-it’s about how your aging body handles each one.What Doctors Should Do-And Often Don’t
The Beers Criteria, updated in 2019, gives clear guidance: start seniors on 20-40% lower doses of liver-metabolized drugs. For those over 75, reduce even more. But many doctors still prescribe based on age alone, not function.- Always check GFR-not just creatinine.
- Use the CKD-EPI equation, not the old Cockcroft-Gault with race adjustments.
- Review every medication every 6 months. Ask: Is this still necessary? Can it be lowered?
- Watch for drug interactions. A common cold medicine with diphenhydramine can interact with antidepressants and cause delirium.
- Use tools like STOPP/START criteria. Studies show using them cuts adverse events by 22%.
There’s also a growing push for personalized dosing. The FDA approved GeroDose v2.1 in 2023-a software tool that simulates how a drug will behave in an individual based on age, liver enzymes, kidney function, weight, and other meds. It’s not everywhere yet, but it’s coming. The future isn’t “one size fits all.” It’s “one size fits you.”
What You Can Do as a Patient or Caregiver
You don’t need to be a doctor to protect yourself or a loved one. Here’s what works:- Keep a written list of every pill, supplement, and OTC drug you take-including aspirin, ibuprofen, and sleep aids.
- Ask your pharmacist: “Is this dose right for my age and kidney/liver health?” Pharmacists are medication experts-and they’re often the first to spot problems.
- Don’t assume “natural” means safe. Herbal supplements like St. John’s Wort or ginkgo can interfere with blood thinners and blood pressure meds.
- Get a GFR test if you’re over 65 and on any chronic medication. It’s a simple blood and urine test.
- If you feel dizzy, confused, or unusually tired after starting a new drug, don’t wait. Call your doctor. It might be the medication.
There’s no magic pill to reverse aging. But we know how to adjust for it. The tools exist. The science is clear. What’s missing is awareness-and action.
Why This Matters Now More Than Ever
By 2050, 1 in 5 Americans will be over 65. Globally, the number of seniors will double. The cost of preventable hospitalizations from bad drug reactions? $30 billion a year in the U.S. alone. That’s not just money. It’s lost independence. Lost time. Lost life.It’s not about slowing aging. It’s about treating older adults with the same precision we use for younger people. We don’t give a 10-year-old the same dose as a 40-year-old. Why do we give a 75-year-old the same dose as a 55-year-old?
The answer isn’t more drugs. It’s smarter dosing. Better monitoring. And listening to the body-not just the calendar.
Do all older adults process drugs the same way?
No. Two 80-year-olds can have very different liver and kidney function. One might have normal GFR and healthy enzyme activity. Another might have severe decline due to diabetes, high blood pressure, or past alcohol use. Age alone doesn’t predict how a drug will behave. That’s why individual testing-like GFR and liver enzyme panels-is critical.
Can I just lower my dose on my own?
Never. Reducing a dose without medical guidance can be dangerous. Some drugs, like blood thinners or seizure medications, need to stay within a narrow range. Too little can cause clots or seizures. Too much can cause bleeding or toxicity. Always talk to your doctor or pharmacist before changing anything.
Why do some seniors need higher doses of certain drugs?
It’s rare, but it happens. Some older adults have very high body fat and low muscle mass, which affects how drugs are distributed. Others may have developed tolerance to a drug over time. In cases like chronic pain or depression, doctors may need to adjust doses upward-but only after checking liver and kidney function, and never without monitoring.
Are herbal supplements safe for older adults?
Not necessarily. Many herbal products interfere with drug metabolism. St. John’s Wort can reduce the effectiveness of blood thinners, antidepressants, and even birth control. Ginkgo can increase bleeding risk when taken with aspirin or warfarin. Turmeric can affect liver enzymes. Always tell your doctor what supplements you’re taking-even if you think they’re “natural.”
What’s the best way to track medication changes?
Use a simple medication log: write down the name, dose, time, and reason for each pill. Bring it to every appointment. Use a pill organizer with alarms if needed. Ask your pharmacist to review your list every 6 months. Many pharmacies offer free med reviews. Take advantage of them.

Brooks Beveridge 15.12.2025
Man, this hit home. My dad was on 5 meds last year and ended up in the ER for 'mystery confusion'-turned out it was the benzo he’d been taking for 10 years. Docs just kept saying 'it's aging.' Nah. It's laziness. We gotta stop treating seniors like broken machines that just need more parts. We need to tune them. Like a classic car-you don’t throw more gas at it when it sputters. You check the carburetor.
And honestly? Pharmacists are the real MVPs here. I wish more people knew to ask them before the doctor.
Love that GeroDose thing. Finally, tech that doesn’t just sell ads.
Anu radha 15.12.2025
My mom took Tylenol every day for back pain. She didn’t know it could hurt her liver. Now she only takes half, and she feels better. Thank you for saying this. So many people don’t know.
Sachin Bhorde 15.12.2025
Bro, this is pure gold. Liver CYP450 isoforms? GFR decline? First-pass metabolism? All underappreciated. Most docs still use Cockcroft-Gault with race correction like it’s 2009. CKD-EPI is the future, no cap. And prodrugs? Perindopril’s a sneaky one-converts to perindoprilat, but if CYP3A4 is down, you get subtherapeutic levels until you double the dose… then boom, angioedema. Been there. Seen that.
Also, acetaminophen >2600mg/day in seniors? That’s a silent killer. Even 3g is risky. Gotta check LFTs. And no, 'natural' supplements ain’t safe-St. John’s Wort induces CYP3A4 like a damn enzyme tsunami.
STOPP/START criteria? Use it. Every 6 months. Your grandma will thank you.
Jane Wei 15.12.2025
So… my grandpa’s on 12 pills. And he’s fine? Or is he just lucky? 🤔
Nishant Desae 15.12.2025
I just want to say thank you for writing this because I’ve seen so many elderly people suffer from what you described, and honestly, it breaks my heart. My aunt was prescribed metformin even though her creatinine was 'normal'-but she’s 81, 98 pounds, no muscle mass. Her GFR was 38. She got lactic acidosis. We almost lost her.
Doctors don’t always know this stuff, and sometimes they’re too rushed to dig deeper. But pharmacists? They’re the unsung heroes. I started taking my uncle’s med list to the pharmacy every six months, and they caught three drugs that were dangerous together. One was a cold medicine with diphenhydramine-he was nodding off all day. They switched him to a non-sedating antihistamine. He’s been sleeping better and walking without a cane since.
It’s not just about age. It’s about your body’s actual function. And if you’re over 65 and on meds, you deserve to have your liver and kidneys checked-not just your blood pressure. Please, don’t wait for a crisis. Ask for a GFR test. Bring your list. Talk to your pharmacist. You’re not being annoying-you’re being smart. And your future self will thank you.
Jody Patrick 15.12.2025
US healthcare is broken. Other countries fix this. We don’t.
Radhika M 15.12.2025
My mom’s doctor didn’t know about the 2600mg Tylenol limit. I told him. He said 'huh, didn’t know that.' So I printed the FDA page. He changed her dose. Small win.
Erik J 15.12.2025
Interesting. But how much of this is just placebo effect from people thinking they're 'old'?
Brooks Beveridge 15.12.2025
Bro, you really just asked if aging is a placebo?
My dad’s liver is 30% smaller. His GFR is 42. His enzymes are slower. That’s not a mindset. That’s a CT scan and a blood test. You wanna argue biology? Go find a hepatologist. Or better yet-go ask your 80-year-old uncle why he fell last week. He didn’t 'think' he was dizzy. His blood pressure dropped because morphine built up.
Some people don’t get it. That’s fine. But don’t dismiss science because it’s inconvenient.
Raven C 15.12.2025
While the sentiment is… *admirable*, I must point out that the reliance on 'GeroDose v2.1'-a software tool with negligible peer-reviewed validation-is emblematic of the dangerous conflation of algorithmic convenience with clinical rigor. The Beers Criteria, while imperfect, are at least evidence-based. To suggest that computational simulation supersedes physician judgment without longitudinal outcomes data is, frankly, reckless. Moreover, the casual dismissal of creatinine-based estimation-despite its widespread utility in resource-limited settings-is elitist and impractical. This piece reads less like medical guidance and more like a Silicon Valley pitch deck dressed in clinical jargon.
Donna Packard 15.12.2025
Thank you for sharing this. I’ve been nervous about my mom’s meds for years. Now I know what to ask. I’ll bring her list to the pharmacist next week. 💙