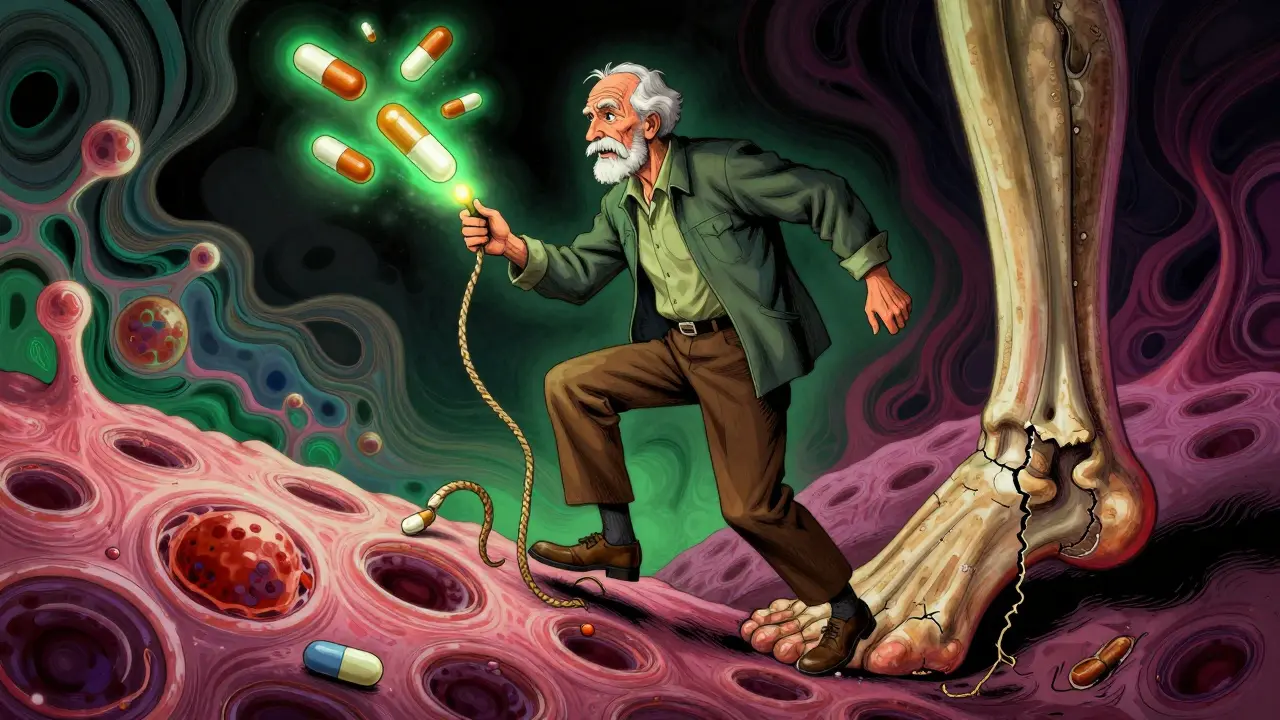
When you’re prescribed an antibiotic for a stubborn infection, you expect relief-not a sudden, painful snap in your heel. Yet for some people, especially those taking both quinolone antibiotics and corticosteroids, that’s exactly what can happen. Tendon rupture, particularly of the Achilles tendon, is a rare but devastating side effect tied to this drug combination. It doesn’t come with warning signs you can ignore. And once it happens, recovery takes months-sometimes years.
What Are Quinolone Antibiotics?
Quinolones, especially the fluoroquinolone subclass, are powerful antibiotics used for serious infections like pneumonia, complicated urinary tract infections, and kidney infections. Common examples include ciprofloxacin (Cipro), levofloxacin (Levaquin), and norfloxacin. They work by blocking bacterial enzymes needed to copy DNA, effectively killing the infection. For decades, they were go-to drugs because they’re oral, broad-spectrum, and effective.
But behind their effectiveness lies a quiet danger. Since the 1980s, doctors have noticed unusual tendon injuries in patients taking these drugs. By 2008, the U.S. Food and Drug Administration (FDA) issued its first safety alert. In 2013, it upgraded the warning to a black box-the strongest possible-requiring manufacturers to clearly state the risk of tendon rupture on all packaging.
The Achilles Tendon: The Most Vulnerable Target
The Achilles tendon connects your calf muscle to your heel bone. It’s the strongest tendon in the body, but it’s also under constant stress during walking, running, or even standing. That’s why it’s the most common site of rupture when quinolones are involved. Studies show that nearly 90% of fluoroquinolone-related tendon ruptures happen in the Achilles.
What’s worse? These ruptures often occur without warning. People report hearing a loud pop, feeling like they’ve been kicked in the back of the leg, and suddenly being unable to stand on their toes. In many cases, the tendon doesn’t rupture immediately-it weakens over days or weeks. Pain, swelling, or stiffness in the tendon may appear first, sometimes as early as a few days after starting the antibiotic. By the time the rupture happens, it’s often too late to prevent it.
Corticosteroids: The Silent Amplifier
Corticosteroids-like prednisone, methylprednisolone, or even inhaled or injected steroids-are powerful anti-inflammatory drugs. They’re commonly prescribed for arthritis, asthma, autoimmune conditions, and allergic reactions. Many older adults take them long-term. But when combined with quinolones, the risk skyrockets.
Research from the General Practice Research Database shows that taking a fluoroquinolone alone increases the risk of Achilles tendon rupture by about 4 times. But when corticosteroids are added? The risk jumps to 46 times higher than in people taking neither drug. That’s not a small increase. That’s a medical emergency waiting to happen.
Why does this happen? Scientists aren’t 100% sure, but the leading theory is that both drugs damage tendon tissue in different ways. Quinolones interfere with collagen production-the main structural protein in tendons. Corticosteroids suppress inflammation and reduce blood flow to tendons, making them more brittle. Together, they turn a strong, flexible band into a frayed rope.
Who’s Most at Risk?
This isn’t a risk that affects everyone equally. Certain groups face a much higher danger:
- People over 60: Age weakens tendons naturally. Combined with these drugs, the risk of rupture doubles.
- Those on long-term steroids: Even low doses over weeks or months increase vulnerability.
- People with kidney disease: Fluoroquinolones are cleared by the kidneys. If kidney function is poor, the drug builds up in the body, raising toxicity.
- Diabetics: High blood sugar damages connective tissues, making tendons more fragile.
- Those with prior tendon injuries: A history of tendinitis or a past rupture makes recurrence far more likely.
- Organ transplant recipients: These patients often take steroids and are frequently prescribed quinolones to prevent or treat infections.
One study found that 2% to 6% of all Achilles ruptures in people over 60 can be directly linked to quinolone use. That’s not rare. That’s preventable.
When Does It Happen?
Many assume the injury occurs while taking the drug. But here’s the catch: half of all tendon ruptures happen after the antibiotic course is finished. The median time to onset is just 6 days after starting the drug. But symptoms can appear up to 6 months later.
That means if you took ciprofloxacin last month and now feel a dull ache behind your heel, don’t brush it off. It could be the first sign of a rupture coming. And if you’re still on steroids? The danger is still active.
What Do the Drugs Look Like in Real Cases?
Case reports tell the real story. A 72-year-old woman with rheumatoid arthritis took prednisone daily and was prescribed ciprofloxacin for a urinary tract infection. Three days later, she felt a pop while walking to the bathroom. She collapsed. Surgery followed. Months of physical therapy. She never fully regained her balance.
A 68-year-old man with diabetes took levofloxacin for bronchitis and was on low-dose steroids for COPD. He felt minor calf pain but ignored it. Two weeks later, he couldn’t stand on his toes. His Achilles tendon was completely torn.
In New Zealand, between 2007 and 2012, 53 cases of tendon damage were reported to their drug safety agency. Of those, 36 were full ruptures. Ciprofloxacin was responsible for 68% of them. Norfloxacin was next. Levofloxacin was far less common in reports-but still dangerous.
How Do Doctors Respond Now?
Because of the evidence, guidelines have changed. The FDA now says fluoroquinolones should only be used when no other antibiotic will work. That means for simple bronchitis, sinus infections, or uncomplicated UTIs, doctors are supposed to choose safer options like amoxicillin, nitrofurantoin, or trimethoprim-sulfamethoxazole.
For patients over 60 on steroids? Many infectious disease specialists won’t prescribe fluoroquinolones at all unless it’s a life-threatening infection like sepsis or anthrax exposure.
Doctors are now trained to ask three questions before prescribing:
- Are you over 60?
- Are you taking steroids-oral, inhaled, or injected?
- Do you have kidney problems, diabetes, or a history of tendon issues?
If the answer is yes to any of these, they’ll reach for a different antibiotic. And if they must use a fluoroquinolone, they’ll warn patients to stop the drug immediately if they feel tendon pain, swelling, or stiffness.

What Should You Do If You’re on These Drugs?
If you’re currently taking a fluoroquinolone and a corticosteroid:
- Stop moving aggressively. Avoid running, jumping, or heavy lifting. Even walking too much can stress a weakened tendon.
- Watch for pain. If you feel any new ache, swelling, or tightness in your heels, shoulders, or hands, call your doctor. Don’t wait.
- Don’t ignore mild symptoms. Tendinitis often comes before rupture. It’s your body’s last warning.
- Ask about alternatives. Is there another antibiotic that could work? Ask your doctor.
- Don’t quit steroids suddenly. Stopping them abruptly can be dangerous. Talk to your doctor about timing.
And if you’ve already finished your antibiotic course? Stay alert for at least 3 months. The risk doesn’t vanish when the pills are gone.
The Bigger Picture
Fluoroquinolones aren’t going away. They’re still vital for treating serious infections like anthrax, drug-resistant pneumonia, and complicated abdominal infections. But their use has dropped sharply since 2013. Prescriptions for ciprofloxacin in the U.S. fell by over 30% in the five years after the FDA’s black box warning.
Meanwhile, research continues. Scientists are studying how these drugs damage collagen at the cellular level. Some think they trigger oxidative stress in tendon cells or overactivate enzymes that break down tissue. Future versions of these antibiotics may be designed to avoid this effect-but for now, the risk is real.
The takeaway isn’t fear. It’s awareness. These drugs save lives. But they can also change them-permanently. If you’re in a high-risk group, don’t accept them as a default. Ask questions. Push for safer options. And if you feel pain in your tendons? Don’t wait. It could be the difference between walking again and needing surgery.
What If You’ve Already Had a Rupture?
If you’ve had a tendon rupture linked to these drugs, you’re not alone. But you’re also a warning sign for others. Many patients report being told their injury was just “bad luck.” It wasn’t. It was a known, documented reaction.
Report your case to the FDA’s MedWatch program. Your experience helps improve safety for everyone. And if you’re prescribed another antibiotic in the future, make sure your medical record notes your history. That information could prevent another rupture.
Can quinolone antibiotics cause tendon rupture even if I don’t take steroids?
Yes. While the risk is much higher when combined with corticosteroids, fluoroquinolones alone can still cause tendon rupture. Studies show a 4-fold increase in Achilles tendon rupture risk even without steroids. The risk is strongest in people over 60, those with kidney problems, or a history of tendon injury.
How long after stopping the antibiotic can tendon rupture occur?
Up to 6 months. While most ruptures happen within the first month of taking the drug, about half of cases occur after the antibiotic course is finished. This delayed onset is why patients are advised to stay alert for tendon pain for months after stopping the medication.
Are all fluoroquinolones equally risky?
No. Ciprofloxacin (Cipro) is the most frequently reported cause of tendon rupture, followed by norfloxacin. Levofloxacin and moxifloxacin carry risk too, but appear less often in reports. However, all systemic fluoroquinolones carry the FDA’s black box warning, so none should be considered safe.
Is tendon damage from these drugs reversible?
Tendinitis (inflammation) may improve if caught early and the drug is stopped. But a full rupture usually requires surgery and months of rehab. Even then, many patients never regain full strength or mobility. The damage to collagen structure is often permanent.
What are safer alternatives to fluoroquinolones?
For most common infections, alternatives include amoxicillin, doxycycline, nitrofurantoin, trimethoprim-sulfamethoxazole, or cephalosporins like cephalexin. The choice depends on the infection type. Always ask your doctor if a safer option is available, especially if you’re over 60 or on steroids.
What to Do Next
If you’re currently taking a fluoroquinolone and a steroid, talk to your doctor today. Ask: Is this the safest option? Are there alternatives? What symptoms should I watch for?
If you’ve had tendon pain after taking these drugs, document it. Share it with your care team. And if you’ve had a rupture, consider reporting it to the FDA. Your experience helps protect others.
This isn’t about avoiding antibiotics. It’s about using them wisely. When the stakes are this high, knowing the risks isn’t paranoia-it’s protection.

Sazzy De 30.01.2026
I took cipro for a UTI last year and noticed my heel felt weird after day 3. Didn't think much of it till I couldn't stand on my toes. Turned out to be tendinitis. Stopped the drug immediately and it cleared up in 3 weeks. Don't ignore those early twinges. It's not just old people.
Adarsh Uttral 30.01.2026
yo i got cipro for a bad sinus infection and my ankle was achin like crazy. doc said it was just overuse. i was like bro i barely walked. turned out i was lucky it didnt snap. now i ask for amoxicillin first. no more quinolones for me.
Lily Steele 30.01.2026
my mom had a rupture on prednisone and cipro. she's 72. took her 18 months to walk without a cane. i now make sure every doctor knows she's on steroids before they write anything.