Cross-Contamination: What It Is and How It Affects Your Medications
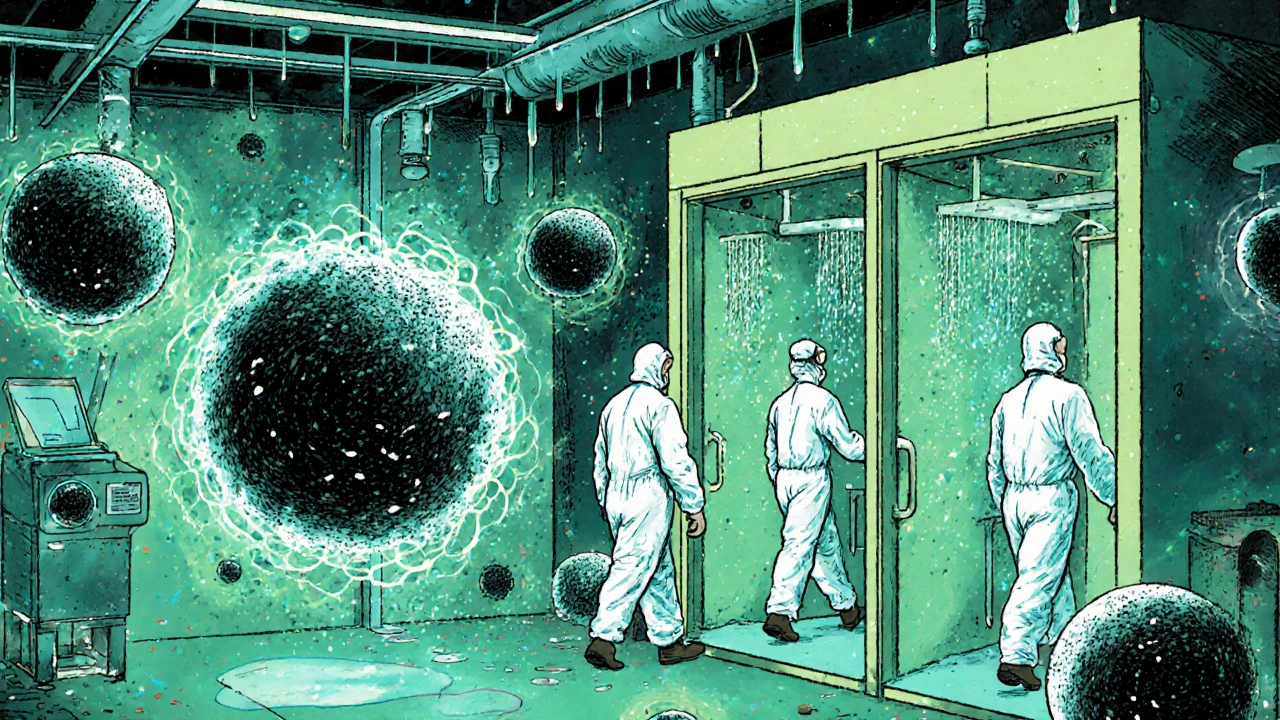
When cross-contamination, the unintentional transfer of substances between medications, surfaces, or containers. Also known as drug mixing, it can turn a safe pill into a health risk—especially when you’re juggling multiple prescriptions, supplements, or over-the-counter drugs. This isn’t just about dirty hands or dusty shelves. It’s about how a crushed tablet in a shared pill organizer can mess with your thyroid meds, how a child’s liquid medicine dropper can contaminate your blood pressure pills, or how a pharmacist’s tool might carry traces of an antibiotic into your antifungal cream.
medication safety, the practice of ensuring drugs are stored, handled, and taken without harmful interference depends heavily on avoiding cross-contamination. Think of your pills like food in a kitchen—if you use the same knife for raw chicken and salad, you risk illness. Same with meds. Iron supplements can stick to the inside of a pill splitter and later mix with your levothyroxine. Antihistamine powder can cling to a grinder used for gabapentin. Even sharing a pill bottle with someone else’s meds can introduce allergens or incompatible chemicals. The drug interactions, harmful chemical reactions between substances that alter their effect you read about? Many start with a simple mix-up you never saw coming.
pill contamination, when foreign substances—dust, moisture, other drugs, or even skin cells—get into your medication is more common than you think. It happens in homes, pharmacies, and even hospitals. A study from the FDA found that nearly 1 in 10 medication errors linked to physical contamination came from shared storage tools. Kids’ chewables left in a drawer can melt and mix with adult pills. Moisture from a bathroom sink can ruin a bottle of pills meant to stay dry. And if you crush pills for ease, you’re creating a powder that can easily spread to other meds in the same container.
People on complex regimens—like those managing kidney disease, thyroid issues, or autoimmune conditions—are most at risk. If you take iron therapy for anemia, or use mesalamine for Crohn’s, or rely on canagliflozin for diabetes, even tiny traces of another drug can throw off absorption, cause side effects, or make your treatment useless. It’s not paranoia. It’s precision medicine 101.
So what can you do? Use separate pill organizers for each drug. Never reuse containers without thorough cleaning. Label everything clearly. Keep liquid meds away from solids. And if you’re splitting pills, use a dedicated tool—don’t share it. Pharmacists can help you get single-dose packaging or blister packs that eliminate mixing entirely.
There’s no magic trick to stopping cross-contamination—just consistent, simple habits. But those habits? They’re the difference between your meds working as they should, and your health taking a quiet, dangerous hit.
Below, you’ll find real-world guides that show you exactly how to protect your meds—from timing iron with thyroid drugs, to reading kids’ labels by weight, to avoiding dangerous mix-ups with common OTCs. This isn’t theory. It’s what works.