Food Allergy Emergency: What to Do When It Strikes
When a food allergy emergency, a sudden, life-threatening reaction to a food trigger. Also known as anaphylaxis, it can turn a simple meal into a race against time. It doesn’t care if you’ve eaten that food ten times before. One bite of peanut, shellfish, or even a hidden ingredient in a sauce can trigger swelling, trouble breathing, or a drop in blood pressure—fast. This isn’t a mild itch or stomach upset. This is your body going into overdrive, and seconds matter.
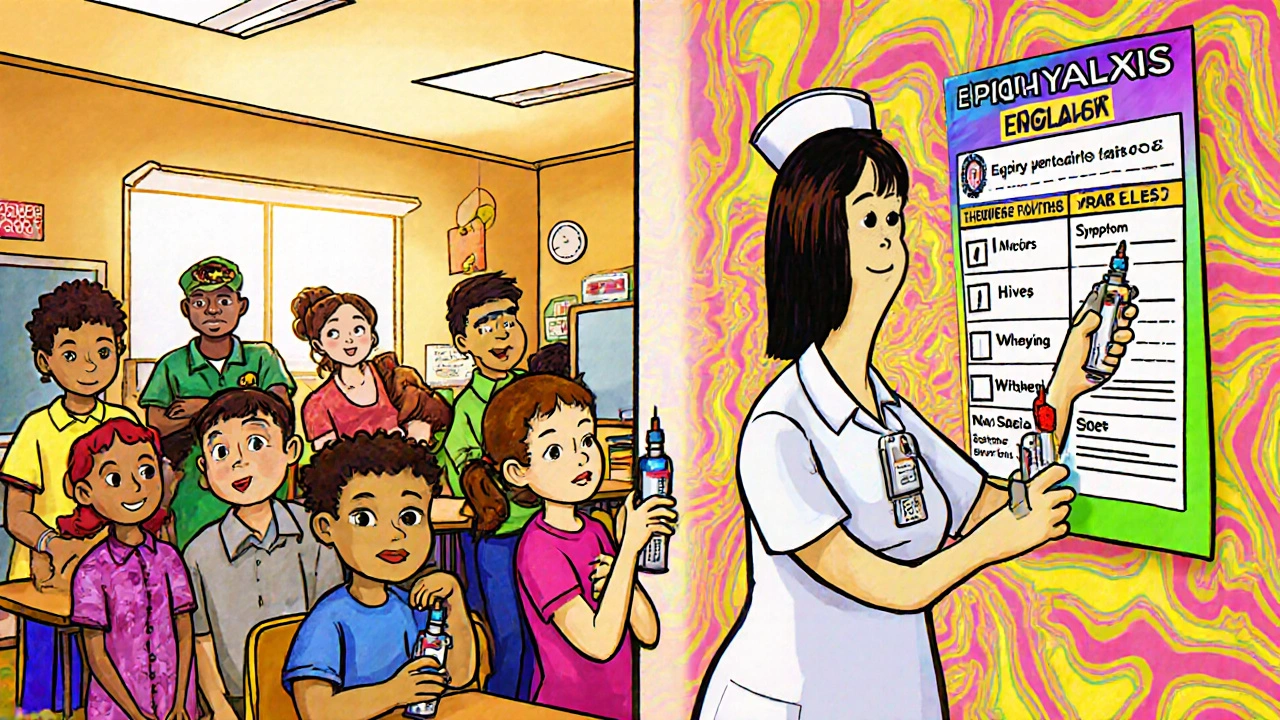
That’s why knowing how to respond isn’t optional. The first and most critical step is using an epinephrine auto-injector, a handheld device that delivers a life-saving dose of adrenaline during severe allergic reactions. If you or someone else is showing signs like throat tightness, wheezing, hives, or dizziness, use it right away—don’t wait. Epinephrine works fast to reverse the reaction, but it’s not a cure. You still need emergency help. Calling 911 after using the injector is non-negotiable. Even if you feel better, symptoms can come back stronger later. Many people don’t realize this, but over half of fatal food allergy reactions happen because epinephrine was delayed or not used at all.
Prevention starts with awareness. A medical alert bracelet, a wearable ID that clearly states your allergies in case you can’t speak. is one of the simplest, most reliable tools you can have. EMTs and hospital staff look for these first in emergencies. Engrave it with your exact allergens—not just "allergic"—and include if you carry epinephrine. Don’t rely on phone notes or wallet cards. In a crisis, no one will think to check your phone. And if you’re traveling, dining out, or sending a kid to school, make sure the people around you know what to do. Teach your family, coworkers, teachers. Practice using a trainer injector. Know where your epinephrine is stored—and that it hasn’t expired.
Food allergy emergencies don’t always come with warning. That’s why having a plan beats hoping for the best. The posts below give you real, practical advice: how to wear your medical ID correctly, what to pack when traveling with allergies, how to read labels for hidden triggers, and why some people react to smells or cross-contact. You’ll find clear guidance on what works, what doesn’t, and how to stay in control—even when the situation feels out of control. This isn’t theory. These are the steps that save lives.