Biosimilars: What They Are, How They Compare to Brand Drugs, and Why They Matter
When you hear biosimilars, highly similar versions of complex biologic drugs made after the original patent expires. Also known as biologic generics, they offer the same clinical benefits as the original but at a fraction of the cost. Unlike regular generics, which are simple chemical copies, biosimilars are made from living cells—making them far more complex to produce. That’s why they’re not exact copies, but close enough to work the same way in your body. The FDA and other global regulators require rigorous testing to prove they match the original in safety, purity, and strength.
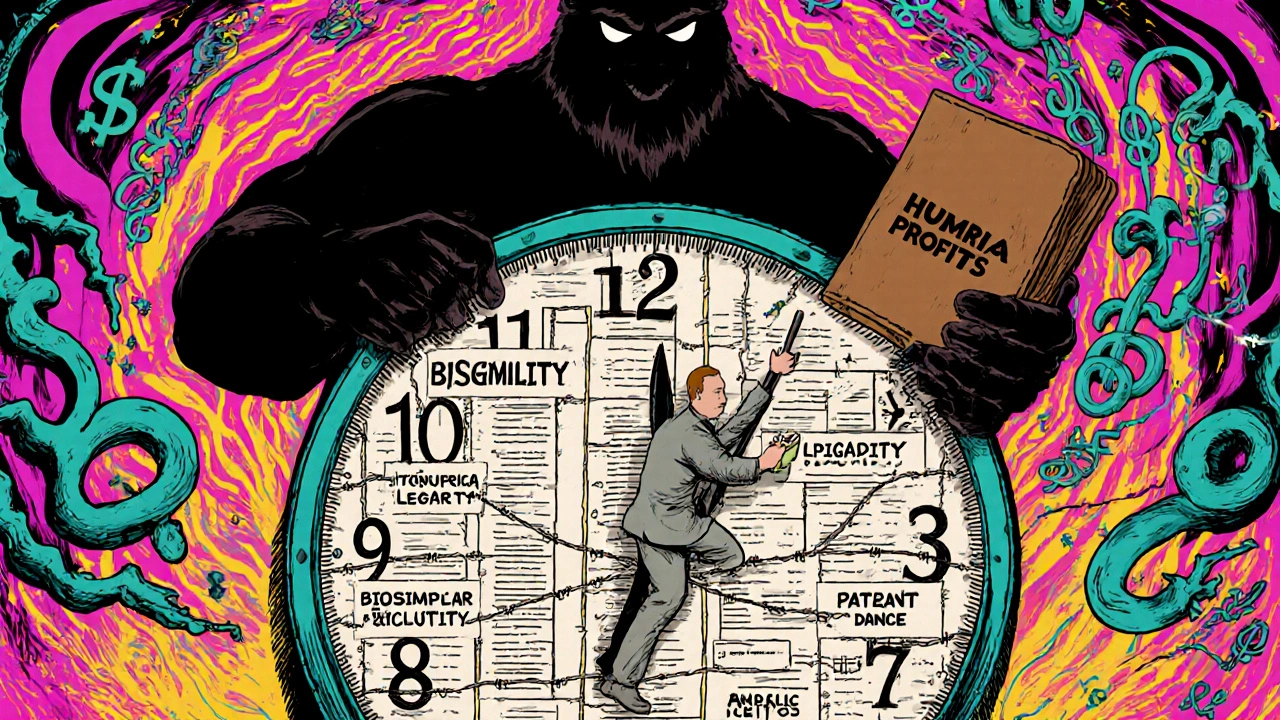
These drugs aren’t just about saving money—they’re changing how people access life-saving treatments. biologic medications, complex drugs made from living organisms, often used for cancer, autoimmune diseases, and chronic conditions like rheumatoid arthritis or Crohn’s disease used to cost tens of thousands a year. Now, biosimilars are bringing those prices down by 20% to 40%, sometimes more. For example, a biosimilar to Humira can cut the cost from $2,000 per month to under $1,200. That’s not a small difference—it’s the difference between staying on treatment or dropping out.
But switching isn’t always simple. generic drugs, simple chemical copies of brand-name pills, approved through faster pathways have been around for decades, and people trust them. Biosimilars are newer, and some patients and doctors still worry—even though studies show no meaningful difference in outcomes. The real issue? Insurance rules, pharmacy substitutions, and confusing labeling. Some plans push biosimilars automatically. Others won’t let you switch without a doctor’s note. And if you’re stable on a brand drug, changing to a biosimilar can cause anxiety, even if it’s medically safe.
That’s why the posts here don’t just explain biosimilars—they show you what actually happens when people switch. You’ll find real stories about medication changes that triggered unexpected side effects, how pharmacies substitute drugs without telling you, and why some people feel worse after switching—even when labs say everything’s fine. We also cover how countries like Germany and Canada use biosimilars to keep their healthcare systems running, while the U.S. still struggles with slow adoption and pricing games. You’ll see how contamination controls in manufacturing, the role of pharmacogenomics, and even mental health reactions tie into this whole system.
Whether you’re on a biologic right now, considering a switch, or just trying to understand why your prescription cost dropped suddenly, this collection gives you the facts without the fluff. No jargon. No hype. Just what you need to know to ask the right questions, spot red flags, and make sure your treatment stays safe and effective.