FDA Exclusivity: What It Means for Drug Prices and Generic Access
When a drug company gets FDA exclusivity, a period of market protection granted by the U.S. Food and Drug Administration that prevents generic versions from entering the market. It's not the same as a patent—this is a separate rule designed to reward innovation, but it often delays cheaper alternatives by years. This means even if a drug’s patent expires, generics still can’t launch until the exclusivity window closes. For patients, that can mean paying hundreds more per month for the same medicine.
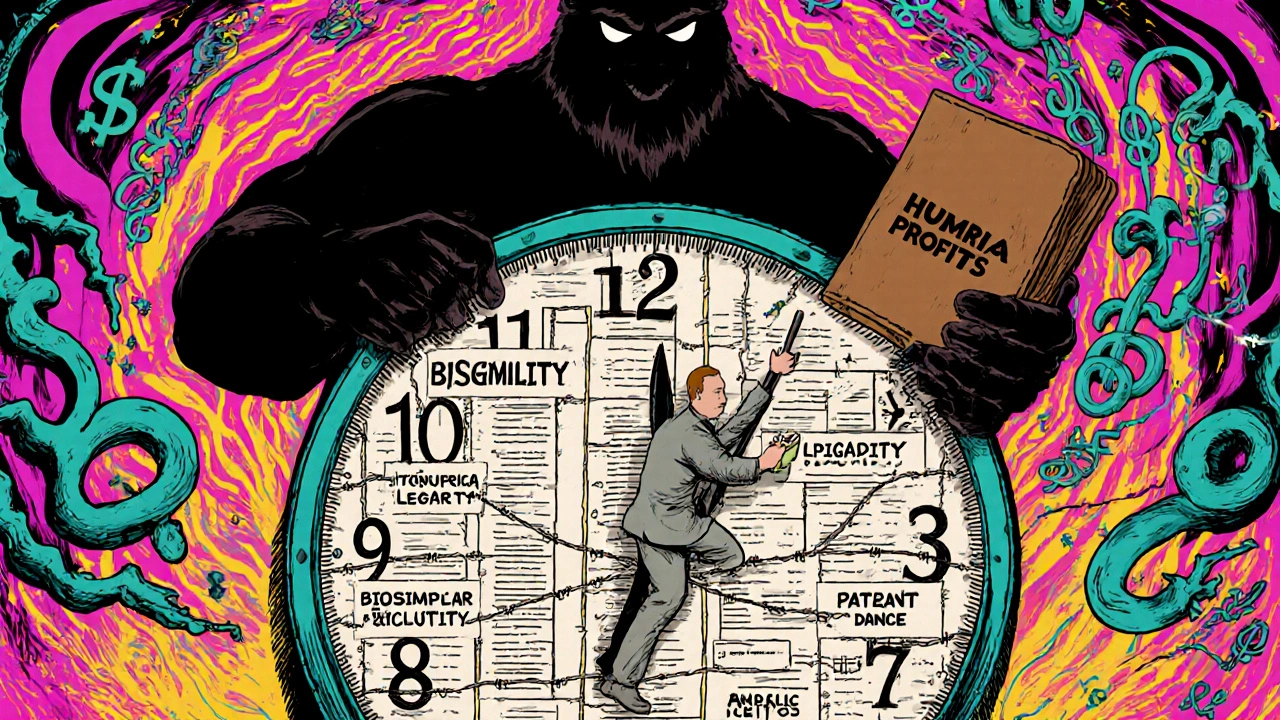
FDA exclusivity applies to different types of drugs in different ways. Orphan drugs, medications for rare diseases affecting fewer than 200,000 Americans get seven years of exclusivity. New chemical entities, drugs with active ingredients never approved before get five years. And if a company does new studies for kids, they get an extra six months. These rules sound fair on paper, but they’re why drugs like Humira or EpiPen stayed expensive for over a decade after their patents ran out.
The connection between exclusivity and generic availability is direct: no exclusivity, no delay. That’s why you’ll see posts here about how generic drugs finally hit the market after exclusivity ends, how pharmaceutical market shifts when competition kicks in, and why some patients can’t access affordable versions until years later. You’ll also find real-world examples—like how FDA approval timelines interact with exclusivity, or how drug makers use loopholes to extend their control. This isn’t theory. It’s about what’s in your pill bottle and what’s on your pharmacy receipt.
What you’ll find below are posts that dig into how exclusivity impacts real people—whether it’s the timing of a generic thyroid med, the cost of switching psychiatric drugs, or why a life-saving injection stays expensive long after its patent dies. These aren’t abstract policy debates. They’re stories about access, affordability, and the hidden rules that decide who gets treated—and who waits.