Pharmacogenomics Testing: How Your Genes Affect Your Medications
When you take a pill, your body doesn’t treat it the same way everyone else’s does. That’s because of pharmacogenomics testing, the study of how your genes influence how your body processes drugs. Also known as gene-drug testing, it explains why one person gets side effects from a common painkiller while another feels nothing, or why someone needs twice the dose of an antidepressant to feel better. This isn’t guesswork—it’s science built on your DNA.
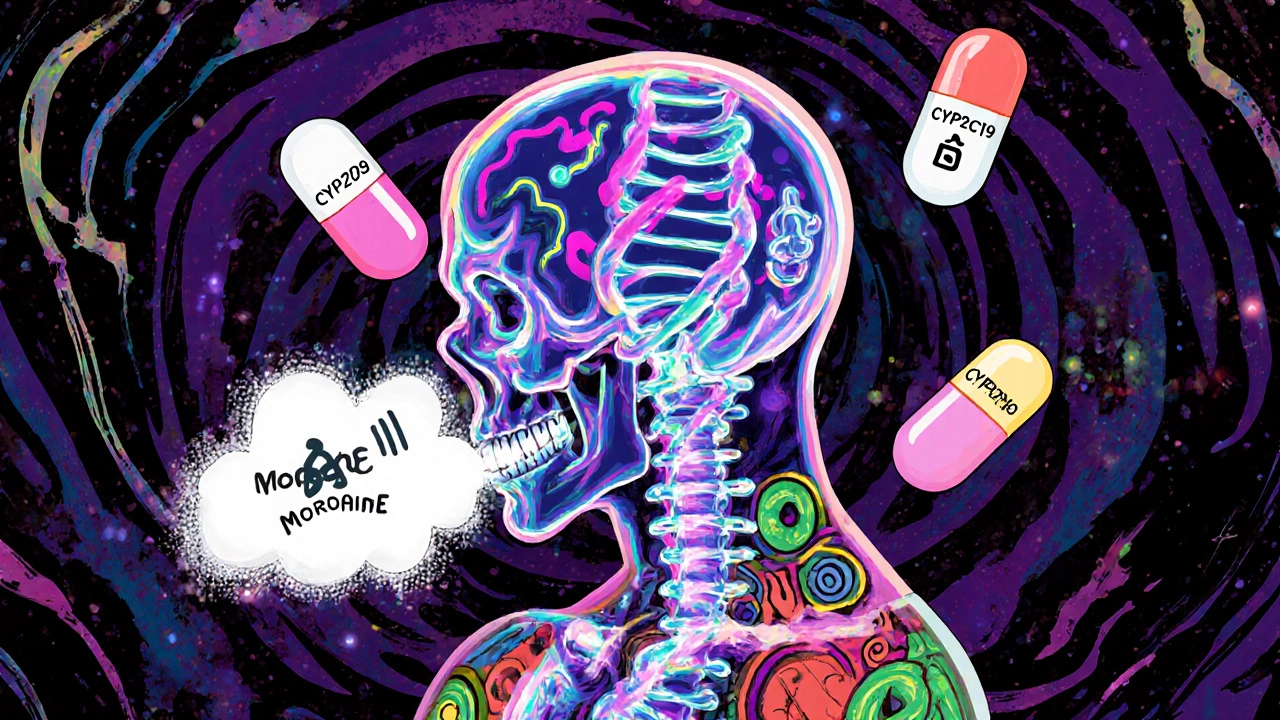
Pharmacogenomics testing looks at specific genes that control how your liver breaks down drugs, how your cells absorb them, and even how your brain responds to them. It’s not about predicting disease—it’s about predicting response. For example, if you carry a variant in the CYP2D6 gene, you might process codeine too slowly (so it doesn’t work) or too fast (so it turns toxic). Or if you have a variant in the HLA-B*15:02 gene, taking carbamazepine could trigger a life-threatening skin reaction. These aren’t rare cases. Studies show over 90% of people carry at least one gene variant that affects how they respond to one or more common medications.
This isn’t just for psychiatrists or oncologists. It matters if you’ve ever been told a drug "didn’t work" for you, or if you’ve had side effects others didn’t. It matters if you’re on multiple medications and feel like your body is fighting them. Pharmacogenomics testing helps explain why. It connects the dots between your biology and your treatment. And it’s not science fiction—it’s already being used in hospitals and clinics to avoid dangerous reactions and find the right drug faster.
Related to this are personalized medicine, tailoring treatment based on individual genetic, environmental, and lifestyle factors, and genetic drug response, how your inherited traits determine whether a medication will be effective or harmful. These concepts are the foundation of modern prescribing. You wouldn’t give someone with a peanut allergy a peanut butter sandwich. Why give someone a drug their genes tell you will fail—or hurt them?
The posts below cover real-world cases where genetics quietly shape treatment outcomes: how thyroid meds interact with iron, why switching antidepressants can trigger emotional crashes, how kidney disease drugs need careful dosing, and why some people react badly to common OTC painkillers. These aren’t random stories. They’re clues pointing to a bigger truth: your genes are already writing your medication story. Pharmacogenomics testing just helps you read it.