Medication Safety and Drug Interactions in November 2025: What You Need to Know
When it comes to medication safety, the practice of using drugs correctly to avoid harm while achieving therapeutic goals. Also known as drug safety, it’s not just about taking pills as directed—it’s about understanding how your body reacts to them, what they mix with, and who’s responsible for keeping them clean and effective. In November 2025, the focus shifted hard to real-world risks: contaminated generics, hidden interactions, and how even small changes in timing or brand can break your treatment.
One major thread running through the month’s articles is generic drugs, lower-cost versions of brand-name medications approved by the FDA as therapeutically equivalent. Also known as substitutable medications, they save billions—but they’re not always as simple as they seem. From therapeutic equivalence codes, FDA labels that tell you if a generic can safely replace a brand drug to nitrosamine contamination scandals that triggered over 500 recalls since 2018, the system is under pressure. Patients aren’t just guessing—they’re learning how to read labels, ask pharmacists the right questions, and spot when a switch might hurt more than help.
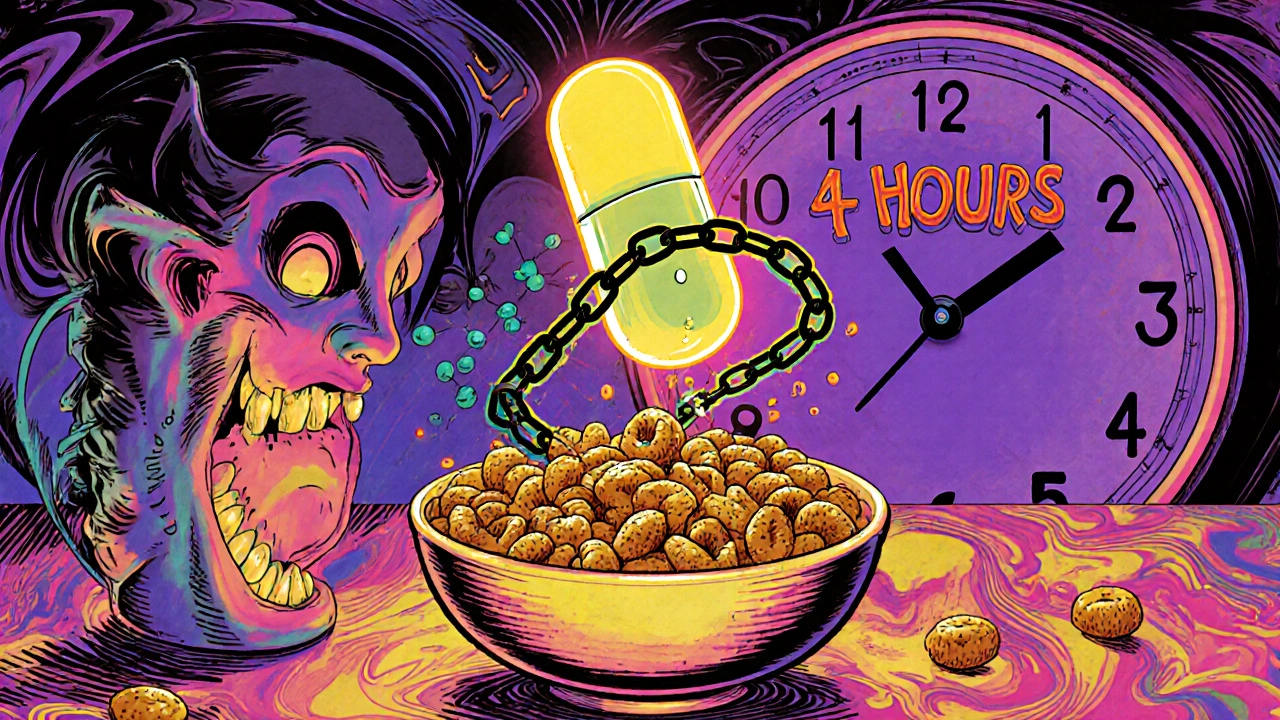
Then there’s the silent danger: drug interactions, when one medication changes how another works in your body. Grapefruit juice turning simvastatin into a muscle-damaging toxin. Iron-rich meals blocking thyroid meds. Antidepressants causing night sweats so bad you can’t sleep. These aren’t rare edge cases—they’re everyday traps. And the fixes? Simple timing rules, like waiting four hours between iron and levothyroxine, or knowing which statins won’t react with citrus. It’s not about avoiding medicine—it’s about using it smarter.
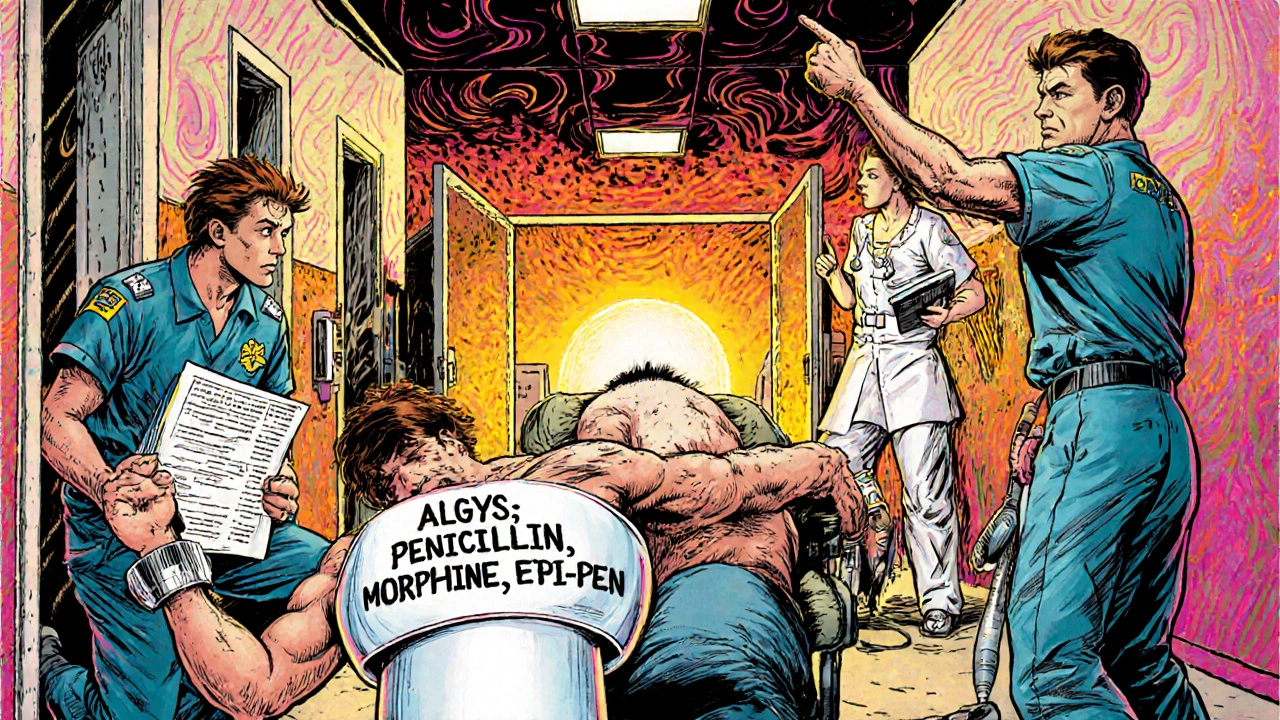
Behind every interaction, every recall, every switch is a system trying to keep up. The BPCIA, the law that blocks biosimilars from entering the U.S. market for 12 years keeps prices high. Contamination controls in manufacturing plants are tightening, but human error still slips through. Even something as basic as a medical alert bracelet, a wearable ID that tells emergency responders about your drug allergies—a tool that costs under $20—can be the difference between life and death. These aren’t abstract policy issues. They’re personal. They affect how you take your pills, how you feel after taking them, and whether you can trust what’s in your medicine cabinet.
What you’ll find below isn’t a list of random articles. It’s a practical guide built by people who’ve been there—parents checking children’s dosing labels, patients switching psychiatric meds and feeling off, someone with kidney disease wondering why their energy won’t bounce back. Every post answers a real question someone asked after a bad reaction, a confusing label, or a doctor’s offhand comment. No fluff. No theory. Just what works, what doesn’t, and what you need to do next.